 The Division of Laryngology within the Department of Otolaryngology – Head and Neck Surgery at The Ohio State University College of Medicine continues to advance research and clinical innovation, leading to improved patient outcomes.
The Division of Laryngology within the Department of Otolaryngology – Head and Neck Surgery at The Ohio State University College of Medicine continues to advance research and clinical innovation, leading to improved patient outcomes.
The division is improving patient access to laryngology surgery services at new clinical sites at The James Outpatient Care and Martha Morehouse Outpatient Care. Additionally, expanded voice services at Ear, Nose and Throat Westerville and Outpatient Care Dublin mean patients have access to world-class care closer to home, including voice exams and speech-language pathology alongside laryngology.
The department is also growing its innovative research through a collaborative model. Laura Matrka, MD, is the research director for the division and hosts monthly meetings with speech-language pathologists, researchers, laryngologists and the division’s clinical fellow to discuss ideas. This approach has increased output for the division.
“Our team brings a robust research approach and is elevating our division nationally as one that is taking clinical scenarios, studying them and applying them across patient populations to help voice, airway and swallowing outcomes,” says Brad DeSilva, MD, director of the Division of Laryngology and clinical professor in the Department of Otolaryngology – Head and Neck Surgery at the Ohio State College of Medicine.
Dysphagia research: retrograde cricopharyngeal dysfunction
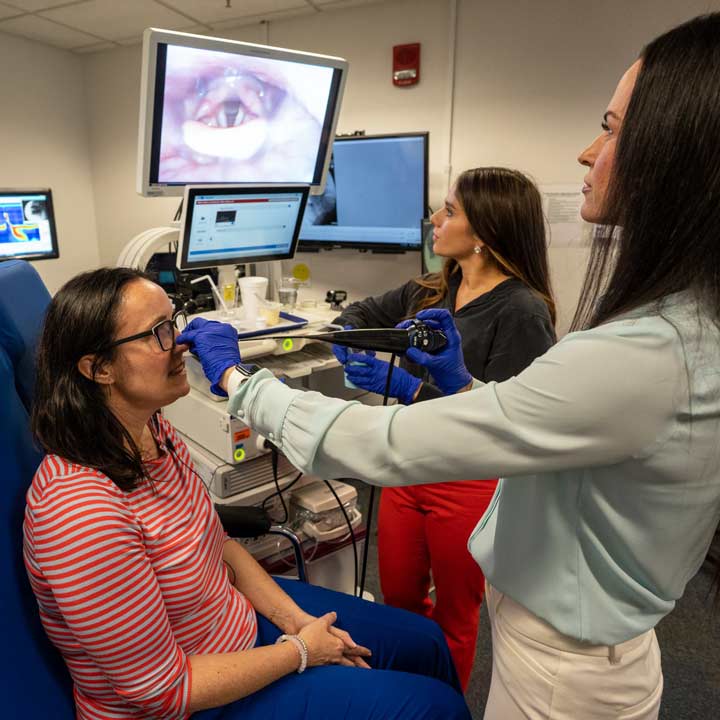
Apoorva Ramaswamy, MD, clinical assistant professor of Otolaryngology – Head and Neck Surgery, is building on her innovative research in dysphagia and breaking ground in the field of retrograde cricopharyngeal dysfunction, a condition that prevents patients from being able to eructate.
“This pathology is one that we’re only coming to recognize in the last five years, especially in younger populations,” Dr. Ramaswamy says.
Through her research, she has pioneered flexible endoscopy for Botox injections in this patient population, which allows them to avoid general anesthesia.
“Many patients have described the discomfort of not being able to eat a full meal,” Dr. Ramaswamy says. “Now, these patients are more comfortable and can enjoy their diet again. We have only known about this condition for a short time, but this intervention is well tolerated for now, and we’re optimistic about long-term patient outcomes.”
Recruiting world-class talent
The Division of Laryngology, in collaboration with the Division of Head and Neck Cancer, recently recruited world-renowned dysphagia researcher Emily Plowman, PhD, who will continue her research across neurogenic and cardiothoracic patient populations.
“Adding Dr. Plowman to our team expands our research expertise in highly innovative areas like dysphagia and other topics in laryngology,” Dr. DeSilva says. “We are looking forward to seeing where her work takes our division in the next couple of years.”
Dr. Plowman has forged a new partnership with Dr. Ramaswamy, given their mutual interests in dysphagia. Their first collaboration examined patient outcomes following balloon dilation procedures in the division’s dysphagia clinic, revealing significant improvements in both airway safety and patient-reported swallowing function after this procedure. Given the lack of historical treatment efficacy data, these will provide important foundational data to guide treatment planning.
“We have been excited to see how people’s lives are improving because of these procedures,” Dr. Ramaswamy says. “People who were aspirating are no longer aspirating. We are showing that there are real, objective improvements in swallowing functions from balloon dilations and other interventions.”
Looking ahead, the pair are planning clinical trials to examine the impact of behavioral, pharmacologic, exercise-based and surgical interventions to improve swallowing outcomes.
“Given that dysphagia is a complex disorder, the conceptualization and implementation of truly translational clinical research is best achieved through team science,” Dr. Plowman says. “When clinical scientists of different backgrounds and mindsets work together toward the common goal of improving patient outcomes — that’s when the magic truly happens.”
As a tertiary referral center with high patient volume, The Ohio State University Wexner Medical Center offers the ideal environment for clinician-scientists to conduct translational and impactful research to advance the field.
“The primary factor driving my decision to join the department was the people — who I felt an instant connection with and shared vision for improving dysphagia patient outcomes,” Dr. Plowman says. “The leadership in the department supports, respects and embraces clinician-scientists, and the Wexner Medical Center provides phenomenal access to patient populations to optimize translational research that my lab performs. This was an amazing opportunity to join forces with a growing dysphagia team and to build a multidisciplinary world-class dysphagia center.”
