
Ohio State researchers identify new biomarkers that differentiate Lewy body dementia from Alzheimer’s and Parkinson’s
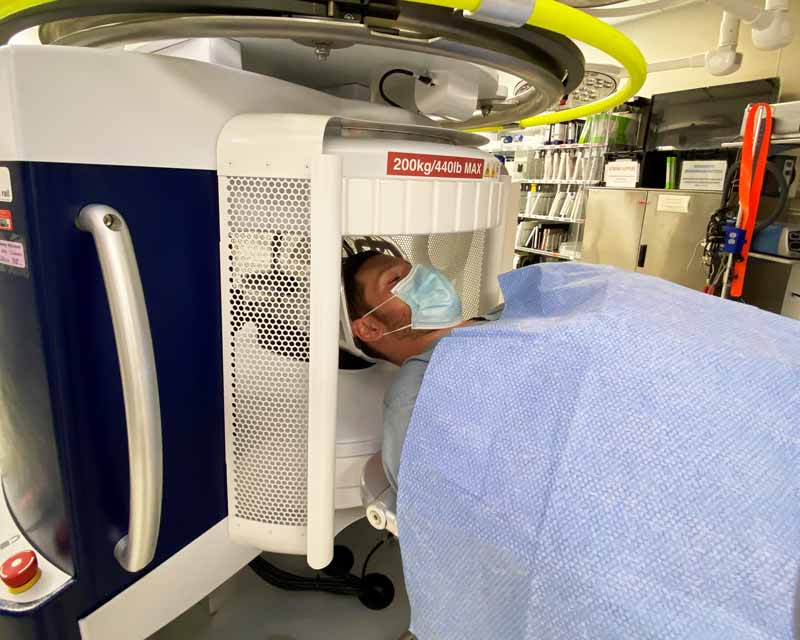
Two new Food and Drug Administration (FDA)-approved Hyperfine Swoop portable magnetic resonance imaging (MRI) devices will vastly improve how quickly doctors at The Ohio State University Wexner Medical Center can assess and treat stroke patients.
These MRI machines make the Ohio State Wexner Medical Center one of the first in the nation — and the only hospital in Ohio — able to evaluate a stroke patient’s brain at their bedside.
“We can utilize this system in multiple time-critical situations ranging from treating stroke patients in the emergency department to performing post-op imaging to ensure an operation has been successful,” says Shahid Nimjee, MD, PhD, a neurosurgeon and surgical director of the Ohio State Wexner Medical Center’s Comprehensive Stroke Center.
The Hyperfine Swoop assesses brain tissue in real time:
“Bringing this technology to the patient’s bedside allows us to provide more patients with acute treatment for ischemic stroke than is currently available,” says Nimjee, who is also an associate professor in The Ohio State University College of Medicine.
A faster patient assessment extends the treatment window for using the clot-busting drug tissue plasminogen activator (tPA). The treatment only works if given up to 4½ hours after a patient began to show signs of having a stroke.
That limits tPA administration nationally to between 5% and 7% of patients among the 800,000 people who present with ischemic stroke each year, Nimjee says.
Most stroke victims don’t receive treatment fast enough to prevent brain tissue damage. The often-irreversible impairment done when a stroke blocks blood flow to the brain includes loss of motor function, paralysis and speech impairment.
Someone in the United States experiences a stroke every 40 seconds. Stroke is also the second-leading cause of death worldwide.
Managing a stroke involves correlating clinical symptoms with brain tissue imaging so that a clot from an acute ischemic stroke can be destroyed and blood flow restored.
“The sooner I can acquire the information, interpret the information and make a decision on how to treat, the better the outcome is for the patient," Nimjee says. “The main goal for our patients is to allow them to return to functional independence.”
Conventional MRIs are large, use a high level of magnetic power and require separate spaces to operate safely. Patients also must undergo a screening for metal detection.
The Hyperfine portable MRI uses a fraction of the magnetic power of a traditional MRI. This lower field strength removes the need for comprehensive patient metal detection and speeds up the screening protocol.
Clinicians can rapidly scan, diagnose and treat patients.
“We simply slide the patient’s head into the head harness and start imaging,” Nimjee says.
As the MRI device scans the patient’s brain, it immediately sends images to the portable viewing screen.
“The neurologist or neurosurgeon can see it, assess the changes and make a clinical decision based on the data in hand,” Nimjee says.
Ohio State expects to achieve multiple benefits from the Hyperfine Swoop MRI.
The device costs less than a traditional MRI unit and saves time and resources by delivering bedside service. The portable MRI also:

Ohio State researchers identify new biomarkers that differentiate Lewy body dementia from Alzheimer’s and Parkinson’s

Biomarker breakthroughs at Ohio State transform disease diagnosis, predictability and treatment

The Ohio State University Wexner Medical Center pushes boundaries for neurological care