
Robotic-assisted surgery with intraoperative radiation offers new hope to patients with local cancer recurrence
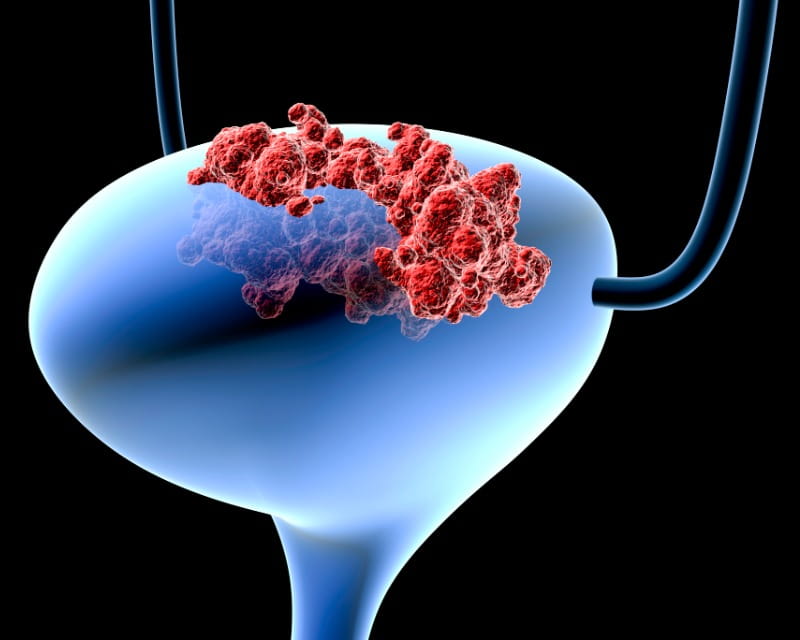 Physician-scientists at The Ohio State University Wexner Medical Center are involved in three promising clinical trials for patients with non-muscle invasive bladder cancer (NMIBC), a group of tumors that tend to have high cure rates followed by high recurrence rates.
Physician-scientists at The Ohio State University Wexner Medical Center are involved in three promising clinical trials for patients with non-muscle invasive bladder cancer (NMIBC), a group of tumors that tend to have high cure rates followed by high recurrence rates.
For many patients with higher-risk NMIBC, the first line of treatment is transurethral resection followed by intravesical therapy using Bacillus Calmette-Guerin (BCG), a live attenuated vaccine that helps prevent cancer recurrence. But a nationwide shortage of BCG – coupled with the fact that many patients fail BCG therapy – means a significant number of people must choose between additional medical therapies with limited efficacy, or radical cystectomy.
With these new studies, eligible patients who prefer to try experimental therapies instead of life-altering surgeries now have several options to choose from.
In order to develop suitable second-line therapies for patients who don’t respond to BCG, Ohio State clinicians are evaluating the safety and efficacy of radiofrequency-induced thermochemotherapy combined with mitomycin C.
“This therapeutic strategy has been used in Europe for over a decade but has not been approved for use in the United States,” says Cheryl Lee, MD, chair of Ohio State’s Department of Urology and holder of the Dorothy M. Davis Chair in Cancer Research at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute. “European data has shown more than 50% of patients who had tumor recurrence following BCG later responded favorably to thermochemotherapy with mitomycin C.”
As part of this industry-sponsored, multi-center study, Ohio State plans to enroll 20 patients who have a type of NMIBC classified as BCG-unresponsive carcinoma in situ (CIS). In addition to tracking complete response rates, Dr. Lee and her team will assess progression-free survival time, bladder preservation rates and overall survival.
“Having access to new intravesical therapies that provide a second line of defense may help more people preserve their bladders,” Dr. Lee says. “If our study results confirm efficacy, thermochemotherapy with mitomycin C could soon be an important alternative for preventing tumor recurrence or progression – which may help people avoid radical surgery and a subsequent decline in their quality of life.”
To learn more about this clinical trial or refer a patient for enrollment, contact Dr. Lee at Cheryl.Lee@osumc.edu.
Ohio State clinicians are also participating in an industry-sponsored, four-arm study that spans 13 countries. It will compare the efficacy of treating BCG-unresponsive NMIBCs with the checkpoint inhibitor nivolumab alone, versus nivolumab in combination with other therapies including an IDO inhibitor and intravesical BCG.
The four arms are designed as follows:
“This study is unique because it’s adaptive,” says site principal investigator Kamal Pohar, MD, associate professor in Ohio State’s Department of Urology and holder of the Julius and Diana Skestos Endowed Chair in Urology. “We’ll confirm safety and efficacy in the first two arms before opening the third and fourth arms, at which point, patients will be randomized to all four arms.”
Dr. Pohar says that while nivolumab is approved only to treat advanced or metastatic bladder cancer, it’s now being tested among patients with earlier stage NMIBCs, including CIS and any T1 or Ta high-grade lesions.
“Checkpoint inhibitors are starting to be evaluated in earlier disease states instead of being restricted to advanced cancers where options are limited,” he explains. “Even though curative therapies already exist for early-stage bladder cancers, we’re hoping the addition of checkpoint inhibitors will bolster outcomes. And further, we’re interested to see whether the IDO enzyme – which is unregulated in many tumors, including bladder cancer – could increase T-cell activity and enhance the effects of nivolumab.”
To refer patients for potential enrollment in this study, please contact Dr. Pohar at Kamal.Pohar@osumc.edu.
In partnership with the SWOG Cancer Research Network, Ohio State began participating in a third clinical trial for patients with high-risk NMIBC in April 2019. The randomized, phase 3 trial has two aims: 1) to test the efficacy of the Tokyo strain of BCG against the currently available Tice strain; and 2) to confirm whether priming with the BCG vaccine prior to intravesical BCG therapy improves response, including recurrence-free survival.
“BCG has been used to reduce cancer recurrence and progression for more than 30 years,” says site principal investigator Debasish Sundi, MD, a urologic oncologist at The Ohio State Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute. “However, given the prevalence of BCG-unresponsive cancers and the current BCG shortage that forces physicians to ration their doses, we must develop intravesical therapies that are more effective.”
To that end, the study team is building off previous research suggesting that some strains of BCG are more effective than others, and that people who had prior exposure to BCG antigens might respond better to BCG treatment.
Dr. Sundi says the trial has a couple of important implications.
“If we prove that the Tokyo strain of BCG is noninferior to the Tice strain, we may help facilitate entry of this strain into the U.S. market and alleviate the current shortage,” he explains. “Second, there is preclinical and clinical evidence to support the notion that people whose immune cells previously processed BCG may have a stronger immune response the next time they receive it. We hope to confirm this by comparing patients who receive standard intravesical BCG only, with patients who receive an intradermal vaccination prior to starting BCG treatment. Ultimately, our efforts could lead to lower rates of disease recurrence.”
To learn more or recommend a patient for enrollment in this clinical trial, please contact Dr. Sundi at D.Sundi@osumc.edu.