 Clinical trials now underway could lead to the approval of the first new therapies for non-muscle-invasive bladder cancer (NMIBC) in more than 30 years.
Clinical trials now underway could lead to the approval of the first new therapies for non-muscle-invasive bladder cancer (NMIBC) in more than 30 years.
Researchers at The Ohio State University Wexner Medical Center — along with those at The Ohio State University Comprehensive Cancer Center – James Cancer Hospital and Solove Research Institute (OSUCCC – James) — are leading multiple studies for this common cancer.
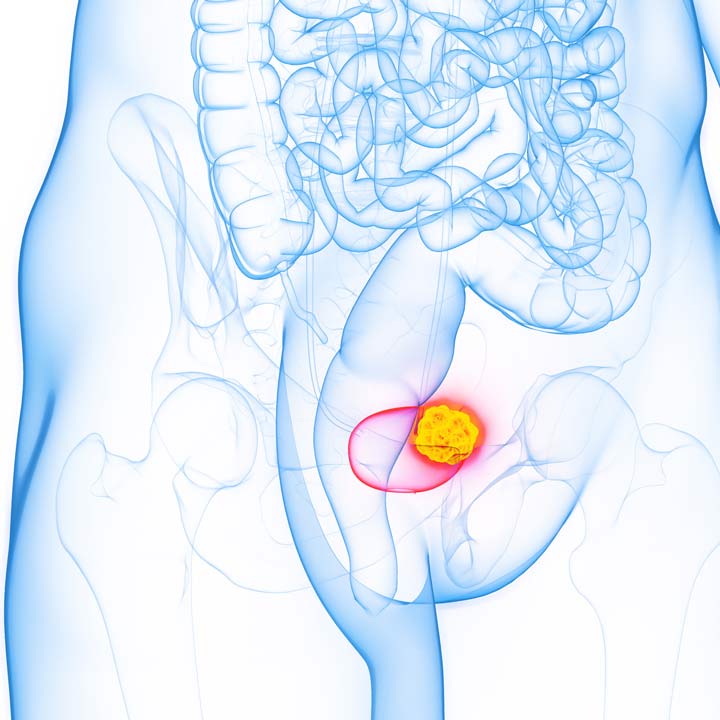
Bladder cancer is the fourth most common cancer in men and the 11th most common cancer in women. Non-muscle-invasive bladder cancer accounts for 75% of all bladder cancers. Experts estimate there were 82,000 new diagnoses in 2023 and 17,000 deaths from the condition.
Radical cystectomy surgery isn’t often recommended for NMIBC. A drug called BCG (Bacille Calmette-Guérin) is the main treatment, Kamal Pohar, MD, says.
“It’s the only option we have worldwide for most NMIBC, and the drug has undergone periods of shortages,” Dr. Pohar says. “It’s not a perfect drug. Some people don’t respond, or it loses its effectiveness. We have opportunities to do better.”
Understanding BCG for bladder cancer treatment
BCG is a bacterium initially created as a vaccine for tuberculosis. Through some serendipity, it was found to have anti-cancer properties.
BCG can be delivered into the bladder by catheter. It works well with few side effects.
Because of its efficacy, BCG became the backbone of bladder cancer therapy.
“It’s such a good, effective drug, it has remained the standard despite all the progress in medicine and cancer treatment,” Dr. Pohar says.
The Ohio State Wexner Medical Center is active in trials within almost every disease space in non-muscle-invasive bladder cancer. Studies are divided into two areas of treatment:
- BCG-naïve, for those newly diagnosed who haven’t used BCG
- BCG-exposed or BCG-unresponsive, for patients who received BCG and didn’t respond to it or saw their cancer return after a short course of treatment
Promising trials underway to treat bladder cancer
Dr. Pohar highlights three promising trials:
A head-to-head comparison with BCG
The cooperative group trial, BRIDGE (A Randomized Phase III Trial of Intravesical BCG versus Intravesical Docetaxel and Gemcitabine Treatment in BCG Naive Non-Muscle-Invasive Bladder Cancer), is a non-inferiority trial comparing intravesical BCG to the combination of two intravesical chemotherapy drugs (gemcitabine and docetaxel). This treatment is for use in BCG-naïve, high-risk NMIBC patients.
The chemo drug combination has shown effectiveness in BCG-unresponsive NMIBC and a phase II BCG-naïve trial. Both treatments are delivered into the bladder by catheter.
This is a randomized National Cancer Institute-supported phase III trial. The OSUCCC – James is one of several institutions leading the studies.
“This trial will provide tremendous knowledge and will move the field forward,” Dr. Pohar says.
Virus-mitigated gene therapy
Another trial focuses on an adenoviral therapy (cretostimogene) to treat BCG-unresponsive patients.
Scientists use a virus to carry a specific gene into the cancer cells. The viral gene therapy stimulates a potent immune response to help destroy the cancer cells. The treatment is delivered into the bladder by catheter. This adenoviral therapy has shown promising results and safety, Dr. Pohar says.
“This is so important for patient care,” Dr. Pohar says. “If traditional therapy fails, we don’t have good salvage treatments.”
This trial will close soon. Dr. Pohar is optimistic that the gene therapy treatment could receive Food and Drug Administration approval and be available to patients within 12 to 18 months.
Androgen-blocking agents
The role of androgen (testosterone) biology is well known in the development of prostate cancer. Debasish Sundi, MD, leads an investigator-initiated study at the Ohio State Wexner Medical Center focused on how androgen biology might impact the development and treatment of bladder cancer.
Bladder cancer occurs more often in men than women. Androgen biology could explain why.
The study, which will open soon, combines BCG therapy with an androgen-blocking agent. The trial will evaluate several biological parameters, including the tumor microenvironment, Dr. Pohar says.
Expanding access to all communities
The Department of Urology works to ensure all patients gain access to clinical trials — and that trials focus on a wide range of participant criteria, Dr. Pohar says.
Researchers at the Ohio State Wexner Medical Center and the OSUCCC – James follow national mandates in this area, including those from the National Cancer Institute. Dr. Pohar and his colleagues provide language access and interpreters to patients who need them.
They also use telehealth to ensure patients who access care through the OSUCCC – James network of rural and affiliate health systems can participate in trials.
“Gone are the days when all clinical trial visits had to be done in person,” Dr. Pohar says. “Now we can do them with telehealth, with the patient at their local provider’s office or in their own home.”
Future studies: Tumor microenvironment
Translational research in the lab also may open doors soon to new bladder cancer therapies. Dr. Pohar and his colleagues are studying how the initial operation required to diagnose non-muscle-invasive bladder cancer might impact the disease course.
Using technology called spatial transcriptomics, scientists are studying the tumor microenvironment to measure how the stress of the surgery affects the cancer cells.
“It’s a novel concept,” Dr. Pohar says. “It’s not been studied before, and we want to know if that surgery contributed to the cancer growth in certain patients.”
