
Robotic-assisted surgery with intraoperative radiation offers new hope to patients with local cancer recurrence
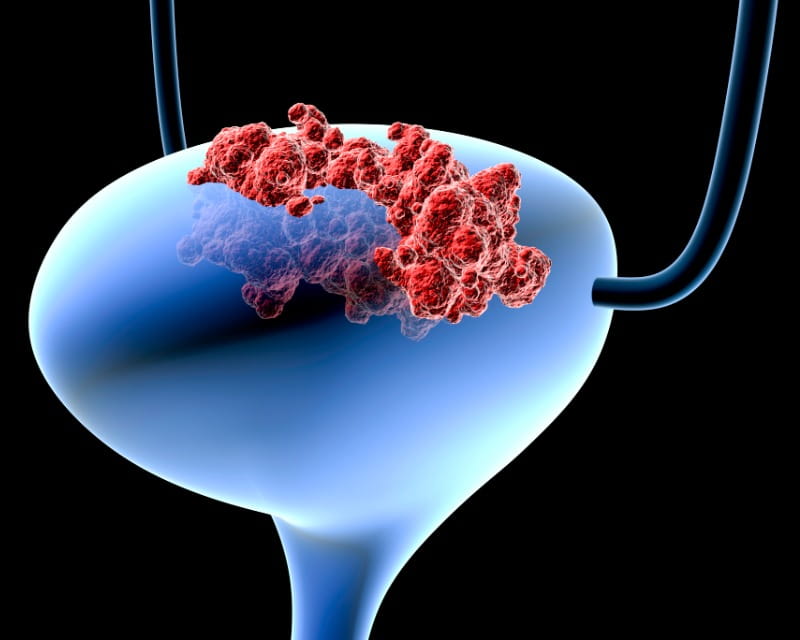 Researchers in the Cancer Biology program at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital (OSUCCC – James) are determined to gain a better understanding of the molecular and cellular changes that occur in the course of bladder cancer development and progression.
Researchers in the Cancer Biology program at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital (OSUCCC – James) are determined to gain a better understanding of the molecular and cellular changes that occur in the course of bladder cancer development and progression.
Debasish Sundi, MD, is one of the pioneering researchers at the forefront of this endeavor. He and his lab are using a new technology known as single-cell RNA sequencing to analyze cell changes that occur from exposure to known bladder cancer-causing agents (carcinogens) and throughout the course of the disease.
Though this study is ongoing, researchers have already gained insight with implications for developing innovative targeted immune therapy treatments. Their findings are also forming the basis for future potentially groundbreaking studies.
Healthy cells are encoded with the information required for normal cell development and functionality. Cancer cells, by contrast, often have multiple signaling pathways that are disturbed — relatively disarrayed compared to healthy cells. The variety of intrinsic subtypes (basal and luminal, for example) affected in bladder cancer adds to this complexity.
Bladder cancer is associated with several risk factors — primarily smoking, but also age, sex and certain environmental or industrial chemicals. Though some risk factors can be modified, others cannot, increasing the urgency to find more effective treatments and prevention strategies.
Current treatment options for bladder cancer include chemotherapy, immunotherapy, surgery and radiation. Dr. Sundi and his team are working to improve medical treatments for bladder cancer that leverage immune cells to counteract cancer cells.
Dr. Sundi’s research, which was funded in part by the American Urological Association (AUA) Urology Care Foundation, is based on a robust mouse model that allows him and his team to analyze the bladder cells of mice from the time of carcinogen exposure throughout the disease process at carefully measured intervals. The genomic patterns of mouse bladders have cellular and molecular features nearly identical to human bladder cancers, making findings from the mouse model generalizable to humans.
With this study, Dr. Sundi has been able to identify early molecular changes in the tumor immune microenvironment providing relevant data to understand cancer development in a whole new way.
“Single-cell RNA sequencing is a genomic technology that can help us to understand cancer cells at a very high level of detail,” Dr. Sundi says. “We can now look at tissue samples with a depth and clarity never before possible.”
Before using this technology, researchers were limited in their ability to differentiate the cell types affected by tumor growth. They were relegated to working with samples measuring the average of all cell types while monitoring tumor growth. “Our current approach gives us the ability to preserve and barcode each cell type,” Dr. Sundi says, “providing the opportunity to trace back gene expression to individual cells, thus increasing the precision of our results.”
Epithelial cells are most often the cell type of origin in bladder cancer. Examining these cells at a molecular level has revealed the upregulation of several oncogenes. This suggests several new druggable targets with the potential to be therapeutically important, Dr. Sundi says. By assessing alterations in the earliest stages of this disease, the potential for limiting disease progression is very promising.
Another important finding is the insight gained related to changes in T cells, a type of cancer-fighting immune cell. Dr. Sundi explains that in the cancer-affected mouse bladders, “over time, T cells had higher and higher levels of molecules that could contribute to T cell exhaustion. Exhausted T cells are not likely to be effective in eradicating cancer cells. In cancer, you want T cells turned on, in their ‘effector’ state. When T cells are overwhelmed early in tumorigenesis, this permits cancer cell growth.”
A related finding involves androgen receptor genes. This is relevant to the sex disparity in bladder cancer. About 80% of bladder cancer cases occur in males. Androgen receptor activity, which tends to be higher in males than in females, was found to be very prominent in tumor-infiltrating T cells. This finding is important because androgen receptor signaling has been linked to T cell exhaustion in prior work done by Dr. Sundi and his collaborators at Ohio State. Additional immunological studies on the biology of sex differences, funded by the Department of Defense, will explore this particular finding in greater detail.