
The Ohio State University Wexner Medical Center expands treatment options for patients with COPD
 New bench research launched at The Ohio State University in 2019 may provide valuable insights about the impact of vaping on lung health.
New bench research launched at The Ohio State University in 2019 may provide valuable insights about the impact of vaping on lung health.
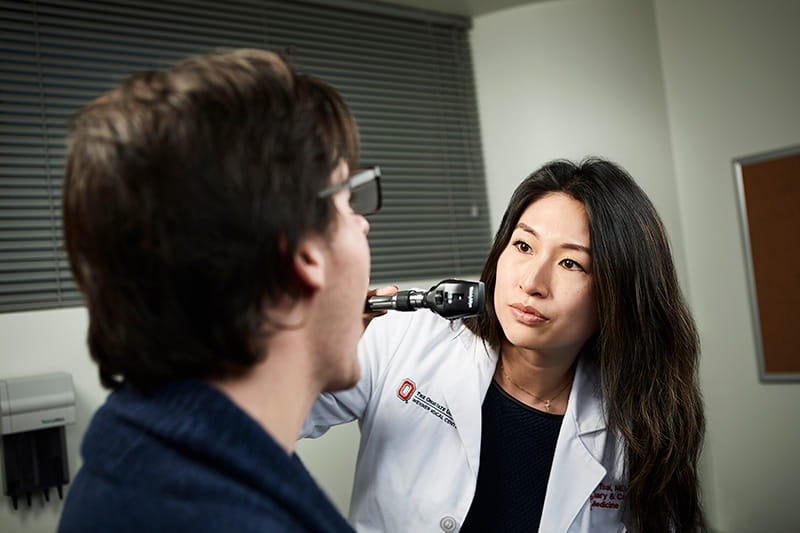
Pulmonologist MuChun Joanna Tsai, MD, a clinical instructor in Ohio State’s Division of Pulmonary, Critical Care and Sleep Medicine, is leading the initiative. Her efforts may shed light on the ability of lung cells to fight infections after exposure to the chemicals found in electronic cigarette (e-cigarette) vapor — and provide evidence that confirms whether vaping poses certain health risks.
Ever since e-cigarettes, vape pens and other battery-powered vaping devices became commercially available in 2007, they’ve been marketed as a safer alternative to traditional cigarettes. Manufacturers also position them as a bridge to smoking cessation.
“While vaping exposes users to fewer chemicals than tobacco cigarettes, the e-liquid in vaporizer products still forms harmful chemicals when aerosolized,” Dr. Tsai says. “The problem is, we don’t know for sure what components and additives may be included in the e-liquids. There are also various vaping devices on the market, with new ones being developed all the time. This has made it difficult to pinpoint the short- and long-term effects of vaping on the respiratory system.”
Additionally, early evidence has shown that vaping is just as addictive as smoking; a single e-cigarette pod or flavor cartridge can contain the same amount of nicotine as a full pack of cigarettes. This means people who attempt vaping as a smoking cessation tool often find themselves with a new habit.
To better understand how vaping affects the lungs, Dr. Tsai, who is an instructor - practice at the College of Medicine, is growing a variety of lung cells in the lab and exposing them to a custom solution extracted from e-cigarette vapor. After applying this vapor extract, she infects the cells with respiratory pathogens to see how they respond.
“My goals with this project are twofold,” Dr. Tsai says. “I’m hoping to gather enough data to apply for a Career Development award through the National Institutes of Health, which would allow me to take this research one step further. Equally important, any evidence we can provide about the effects of vaping on the respiratory or immune systems would help us counsel patients about the validated risks of e-cigarette use.”
Dr. Tsai is also collaborating with other Ohio State investigators to assess the functional effects of e-cigarettes on the lungs.
She and her colleagues, including pulmonologist Mark Wewers, MD, faculty emeritus at the College of Medicine, and lung cancer specialist Peter Shields, MD, a professor at the College of Medicine, recently conducted a small, cross-sectional study of inflammasome protein release in human bronchoalveolar lavage (BAL) fluid. They compared fluid samples from never-smokers, cigarette smokers and people who use e-cigarettes.
Their results, which were published in the American Journal of Respiratory and Critical Care Medicine (April 2019), showed that e-cigarette use may promote the release of the inflammasome adaptor protein ASC into the lungs.
“Previous research has shown elevated ASC in BAL fluid taken from people with chronic obstructive pulmonary disease,” Dr. Tsai says. “Through our study, we found that ASC in BAL fluid was higher in smokers and e-cigarette users when compared with never-smokers.”
Dr. Tsai notes that given the 2019 outbreak of lung injury linked with vaping — which included 47 deaths by the middle of November — symptoms are just as important as scientific evidence.
“We should counsel our patients to stop vaping, especially if they develop symptoms including chest pain, coughing or shortness of breath,” she says. “And for those patients using e-cigarettes as part of their journey to quit smoking, we should advise them to switch to an evidence-based smoking cessation tool as soon as possible.”
Learn more about innovations in care and research from the Division of Pulmonary, Critical Care and Sleep Medicine.