
Robotic-assisted surgery with intraoperative radiation offers new hope to patients with local cancer recurrence
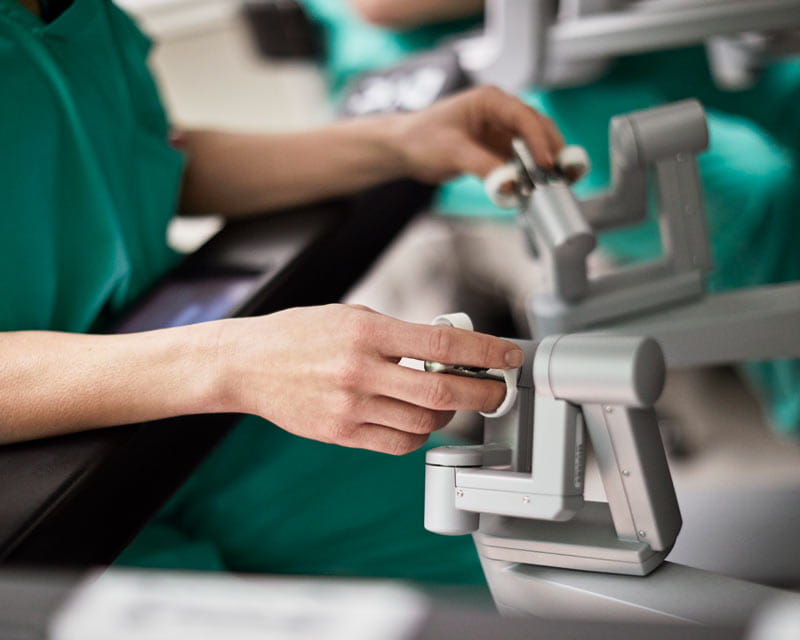 Teaching a resident how to perform a radical nephrectomy or prostatectomy with a robotic surgery system requires patience and skill. But perhaps even more challenging is the task of evaluating each resident’s performance once they take control of the surgical instruments themselves.
Teaching a resident how to perform a radical nephrectomy or prostatectomy with a robotic surgery system requires patience and skill. But perhaps even more challenging is the task of evaluating each resident’s performance once they take control of the surgical instruments themselves.
To address that challenge, urologists at The Ohio State University Wexner Medical Center recently introduced a robotic skills assessment platform that records and measures trainee and trainer performance data during three index urologic robotic procedures. The platform provides objective, actionable feedback to help residents improve their skills and measure their progress over time. It also generates video footage of each procedure, which faculty members can use as a teaching tool.
The platform is a collaboration between Intuitive, maker of the da Vinci robotic surgical system, and urologists at the Ohio State Wexner Medical Center, with support from the Ohio State Center for Advanced Robotic Surgery and Center for Minimally Invasive Surgery.
Urologist Michael Gong, MD, PhD, laid the foundation for the platform by “deconstructing” the three index urologic robotic procedures — prostatectomy, partial nephrectomy and radical nephrectomy — into key components and establishing benchmarks for residents at each postgraduate year level. These objective measures serve as the basis for tracking and measuring trainee performance.
“When attendings train residents in open surgery, we’re right there with them and it’s easier to observe their proficiency and progress,” says Courtenay Moore, MD, a urologist who helped introduce the new platform. “Robotic surgery is different. The resident is on the console and the attending is typically focusing on the video screen. It’s impossible to keep track of how many times the operator is clutching or whether they’re moving the instruments efficiently or taking too long to complete a step. The robot collects and analyzes all that data so that we can provide residents with objective parameters and a standardized assessment.”
Urology residents at the Ohio State Wexner Medical Center do about 400 robotic surgery cases during their five years of training. Most of the surgeries take place at The Ohio State University Comprehensive Cancer Center – Arthur G. James Cancer Hospital and Richard J. Solove Research Institute. Each time residents participate in one of the three index surgeries, the system records data such as how much time each step takes, the number of times the operator clutches and the number of camera movements. After the surgery, the system generates a detailed report highlighting performance metrics related to economy of movement, proficiency, learning curve, operative time, frequency of hand-offs, bimanual dexterity and other markers.
Residents and attendings can view the data on a user-friendly dashboard that highlights information about individual trainees, such as total number of cases, monthly case count and console time by case. They can also see program-level metrics (e.g., surgical volume for different procedures, number of procedures by a faculty member) and navigate to case-specific information.
Moore notes that the new platform allows residents to achieve progressive autonomy as they gain proficiency in specific skills.
“If I haven’t worked with a certain resident for a few months, I need to know what they’re capable of before allowing them to do a certain procedure,” she says. “The platform objectively captures all of that information. So when a resident tells me they can take down a bladder neck, the system can verify how many times they’ve already done it.”
After each surgery, the attending can look at the dashboard with the resident and provide more helpful feedback than was previously possible. “It’s the difference between telling a trainee ‘you did a great job in there’ and ‘you are clutching 40% less than you did four weeks ago,’” Moore says.
Attendings also can use video footage to help residents learn from previous cases by walking through the procedure, making observations, providing guidance for next time and answering questions.
The Department of Urology has plans to harness all of this robotic surgical data to improve resident education overall, says Tasha Posid, PhD, an education specialist and assistant professor of Urology. Posid helps design, implement and assess various curricula in the department, including simulation training.
“With the new platform, we can aggregate cases over time and look at the data by cohort to see, for example, whether all the second-year residents have reached certain benchmarks,” she says. “If not, is there somewhere we need to improve their training to get them to proficiency before their third year? We can also look at the program level for similar metrics and see whether we are producing expert urologic surgeons and identify any gaps we need to address. We will also use this data to develop quality improvement projects that enhance patient outcomes.”
Ohio State is one of nine academic medical centers in the United States. partnering with Intuitive to develop the platform. Other surgical specialties at the medical center are doing similar projects with Intuitive, including General Surgery, Cardiothoracic Surgery and Obstetrics-Gynecology.