2020 Annual Report
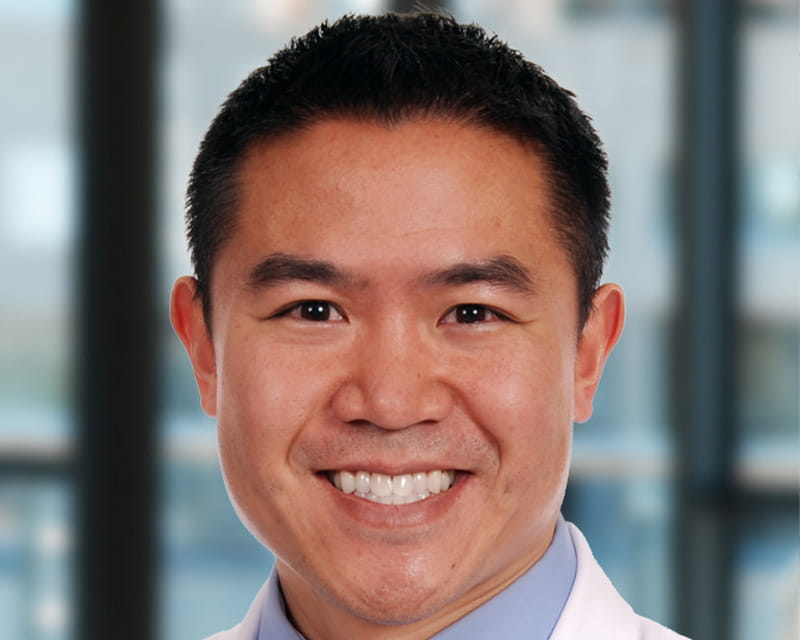 Eugene Chio, MD, was one of the first otolaryngologists in the United States to offer upper airway stimulation therapy for patients with moderate to severe obstructive sleep apnea (OSA). Since 2018, he’s implanted more upper airway stimulation devices than anyone in the world. Dr. Chio continues to refine the procedure, recently reducing the number of incisions needed from three to two.
Eugene Chio, MD, was one of the first otolaryngologists in the United States to offer upper airway stimulation therapy for patients with moderate to severe obstructive sleep apnea (OSA). Since 2018, he’s implanted more upper airway stimulation devices than anyone in the world. Dr. Chio continues to refine the procedure, recently reducing the number of incisions needed from three to two.
Upper airway stimulation therapy, sometimes referred to as “Inspire” after the company that developed it, is an effective option for patients who don’t tolerate CPAP therapy. The implant delivers mild stimulation to the hypoglossal nerve to improve tone and prevent the tongue from blocking the airway. The Food and Drug Administration approved the therapy in 2014, and in 2019, The Ohio State University Wexner Medical Center was designated as an Inspire Center of Excellence—one of about 20 in the world.
“Initial studies show that upper airway stimulation patients experienced a 78% reduction in sleep apnea events, as well as reduced snoring—about 85% of bed partners report no snoring or soft snoring,” says Dr. Chio, director of the Sleep Surgery Program at The Ohio State University Wexner Medical Center.
In addition to helping patients with OSA, this therapy may also be appropriate for patients who have both obstructive and central sleep apnea, as long as the central sleep apnea episodes account for less than 25% of all disrupted breathing episodes.
During an outpatient surgical procedure that typically lasts two to three hours, Dr. Chio makes an incision under the chin to connect a lead to the hypoglossal nerve and another incision below the collarbone to place the battery and the respiratory sensor. Placing the sensor below the collarbone, rather than in the flank, results in needing only two incisions instead of three. Dr. Chio says this allows for a faster procedure and improved healing process, as well as a potentially lower risk of infection.
The device is not activated for the first month to allow for a full recovery. After a month, the patient returns to the Sleep Surgery Center to have the device activated and to set initial stimulation parameters.
The patient uses a handheld remote to turn the device on and off based on their sleep schedule. The device can begin operating at a set interval after going to bed (typically 30 minutes), allowing adequate time for the patient to fall asleep naturally. “The device senses chest wall motion and respiratory effort, issuing stimulation only when the patient inhales, which is when OSA occurs,” Dr. Chio says. “This stimulation moves the tongue forward to prevent airway obstruction. Upon rising, the patient simply turns off the device using the remote.”
Some patients report mild twitching of the tongue during use, but adjusting the stimulation settings can minimize this. The device battery lasts about 11 years and can be replaced when necessary.
Upper airway stimulation is indicated for patients with moderate to severe OSA who have failed conservative therapies, such as CPAP. The therapy is approved for patients with a body mass index (BMI) of less than 32, although patients with a BMI of up to 35 may be eligible. An evaluation for upper airway stimulation includes a drug-induced sleep endoscopy (DISE) to ensure that the patient’s anatomy is compatible with treatment.
Dr. Chio and his colleagues at the Sleep Surgery Center offer other procedures for people with moderate to severe OSA, including tonsil removal, nasal surgery, and a variety of palate surgery/tonsil, soft palate, and tongue-based procedures.