
Safer Patient Transport
 Multi-arterial grafting is becoming the standard approach to coronary artery bypass surgery at The Ohio State University Wexner Medical Center
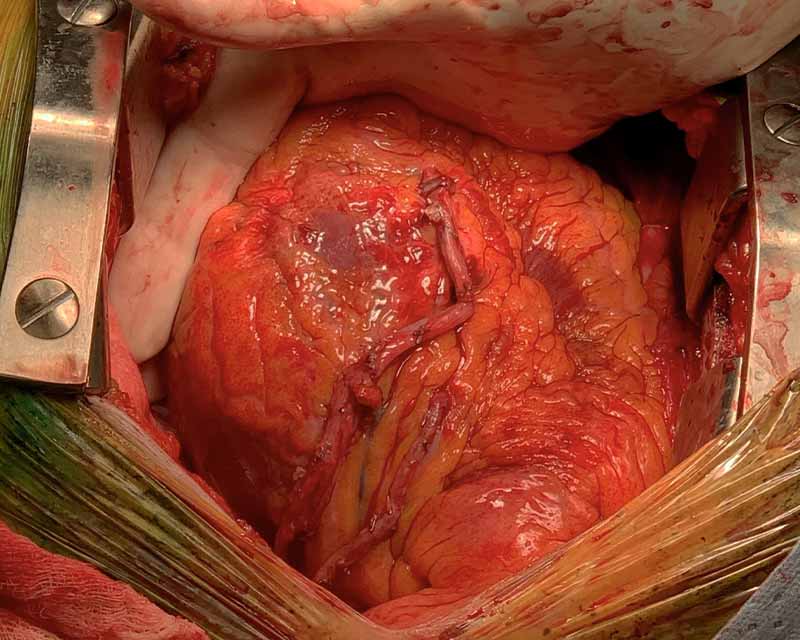
Multi-arterial grafting is becoming the standard approach to coronary artery bypass surgery at The Ohio State University Wexner Medical CenterA growing body of research suggests that bilateral internal thoracic artery (BITA) grafting provides the best outcomes for coronary artery bypass graft (CABG) patients. Armed with this evidence, cardiac surgeons at The Ohio State University Wexner Medical Center are significantly increasing their use of BITA to treat coronary artery disease.
“CABG surgery remains the most common heart surgery in the U.S., accounting for 60% of all heart procedures,” says Nahush Mokadam, MD, professor and director of the Division of Cardiac Surgery at the Ohio State Richard M. Ross Heart Hospital. While most CABG surgeries are performed using single internal thoracic artery (SITA), recent research shows that BITA results in better outcomes.
“The evidence shows that BITA prolongs graft patency, extends survival and reduces the need for further interventions — all goals in the care for patients with heart disease,” Mokadam says. “BITA is performed by all cardiac surgeons at the Ross Heart Hospital.”
Below are the numbers at Ohio State:
It was 1968 when the first arterial graft was performed by suturing the left internal thoracic artery (LITA) to the left anterior descending artery (LAD). For some time, the standard was to use the LITA for the first graft, especially to the LAD, and saphenous vein grafts (SVG) to bypass other coronary artery blockages.
In spite of ongoing advancements, Mokadam says, these SITA graft approaches and associated venous grafting techniques are prone to failure.
Because of that, there has been much experimentation to determine the best vessel for the second and subsequent grafts to improve revascularization of the myocardium and avoid or delay further surgical interventions.
The evolution in grafting has progressed at some centers to the use of BITA, which has been shown to have a 70% survival rate more than 20 years post-CABG.
“The fact that the benefits of multi-arterial grafts continue into the second decade postsurgery is significant,” Mokadam says. “By growing our use of BITA, we’re working to create healthier futures for our patients.”
Despite studies showing the benefits of BITA, there has been ongoing reluctance among cardiac surgeons to use this grafting technique.
Reasons include:
To provide the best care to their patients, Ohio State cardiac surgeons have demonstrated their commitment by using evidence-based medicine to overcome these barriers.
“At Ohio State, we are committed to providing our patients with the highest level of care, with the best possibility for long-term success. As a group, we reviewed the literature, understood the time required and debunked misconceptions. This allowed us to make this approach a priority for our patients,” Mokadam says.
In addition to Mokadam, members of the cardiac surgery team at Ohio State include John Bozinovski, MD, Asvin Ganapathi, MD, Matthew Henn, MD, and Bryan Whitson, MD, PhD.
“As surgeons, we care deeply for our patients — they entrust us with their lives every day. We are responsible to understand the literature, explore cutting-edge techniques and deliver them to our patients. I think you will be hard pressed to find a center with BITA use higher than ours anywhere in the country or even the world,” Mokadam says.

Safer Patient Transport

New treatment for atrial fibrillation
First US Medical Center in Clinical Trial