
Ohio State Researchers Launch NIH-Funded Study on Ozone-Induced Pulmonary Inflammation
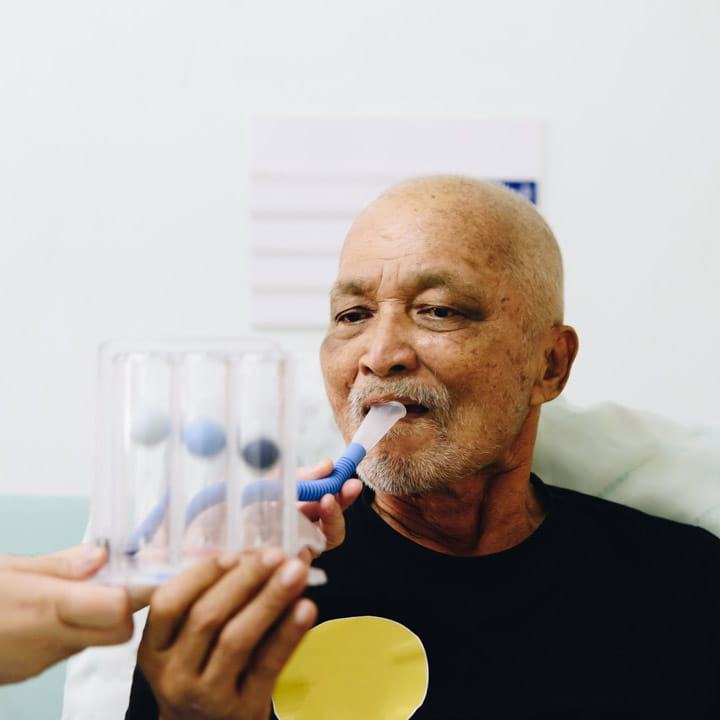 The Ohio State University Wexner Medical Center’s nationally ranked pulmonary rehabilitation program provides a core part of the care for patients with chronic obstructive pulmonary disease (COPD) and other complex lung diseases. Pulmonary rehab is also offered before and after complex procedures like lung volume reduction surgery, bronchoscopic valve placement and lung transplant to improve lung function and health and overall quality of life.
The Ohio State University Wexner Medical Center’s nationally ranked pulmonary rehabilitation program provides a core part of the care for patients with chronic obstructive pulmonary disease (COPD) and other complex lung diseases. Pulmonary rehab is also offered before and after complex procedures like lung volume reduction surgery, bronchoscopic valve placement and lung transplant to improve lung function and health and overall quality of life.
“We have a lot of experience with different diseases throughout the spectrum of lung disease from COPD and pulmonary fibrosis, to sarcoidosis and pulmonary hypertension,” says Philip Diaz, MD, director of Pulmonary Rehabilitation and professor of Internal Medicine in the Division of Pulmonology, Critical Care and Sleep Medicine at the Ohio State College of Medicine. “What makes Ohio State unique is that we have detailed protocols and well-integrated communications, as well as deep experience optimizing outcomes, all with a 25-year track record of working with other programs in the community that are closer to where patients live.”
The team is made up of respiratory therapists, exercise physiologists, pulmonologists, nutritionists, physical and occupational therapists, surgeons, nurses and psychologists.
As part of rehab, patients receive education on their specific condition and how to best manage it, exercise training, energy-conserving techniques, breathing strategies and nutrition counseling. They also have opportunities for psychosocial counseling.
“Education is an important part of a rehab program. We’ve approached education in innovative ways. For instance, in addition to our in-person education sessions, we have also developed remote curricula as a convenient option, especially for patients who live elsewhere,” Dr. Diaz says. “Ohio State also offers a biennial pulmonary rehab conference that many regional rehab programs will attend for education. It helps facilitate sharing of protocols and best practices, and we get to know the other programs as well.”
People with advanced pulmonary disease often experience a high symptom burden, including dyspnea, which can negatively impact their quality of life and result in elevated rates of anxiety and depression.
Researchers led by Kelsey Black, MD, a pulmonary and critical care physician at Ohio State, are exploring how to incorporate mindfulness in pulmonary rehabilitation. In a recent study, a mindfulness-based intervention was offered to people with chronic lung disease participating in pulmonary rehab. Early results suggest that mindfulness may provide a sustained impact in improving perceived stress and self-efficacy. Not only that, but mindfulness group sessions may also be effective in reducing respiratory rates.
“We’re also working on assessments of quality of life — really trying to understand that in a comprehensive way above and beyond the standard,” Dr. Diaz says. “This incorporates multiple dimensions, including emotional and spiritual.”
In an ongoing study, researchers led by Ohio State pulmonary and critical care specialists Kashika Goyal, MD, and Jennica Johns, MD, are applying the Functional Assessment of Chronic Illness Therapy – Palliative Care (FACIT-Pal) survey in a novel way. The 46-item survey is being given to patients with a primary pulmonary diagnosis referred to Ohio State’s Pulmonary Rehab program. The questions are divided by functional domains of living. Preliminary results suggest that people with interstitial lung disease, asthma, pulmonary hypertension and COPD experience different burdens on quality of life. Early findings also support the benefits of pulmonary rehab, as a substantial proportion of people experience a clinically significant increase in their FACIT-Pal score after completing rehab.
Pulmonary Rehabilitation at Ohio State continues to integrate unique facets of care to collaborate and optimize personalized care for this complex and vulnerable patient population.
Learn more about innovations in care and research from the Division of Pulmonary, Critical Care and Sleep Medicine.