March 22, 2023
COLUMBUS, Ohio – More than 1.5 million Americans suffer a traumatic brain injury (TBI) each year, oftentimes resulting in permanent disability, including struggles with memory, mobility, mental health and cognitive function. For those with a TBI, their struggles usually don’t end when treatment does.
An ongoing longitudinal study of 1,400 patients by researchers at The Ohio State University Wexner Medical Center and College of Medicine reveals that traumatic brain injuries don’t stabilize after a couple of years as previously thought.
Instead, as researchers analyzed more than 25 years of data, they found that TBIs need to be treated as a dynamic and chronic condition that requires ongoing resources and care.
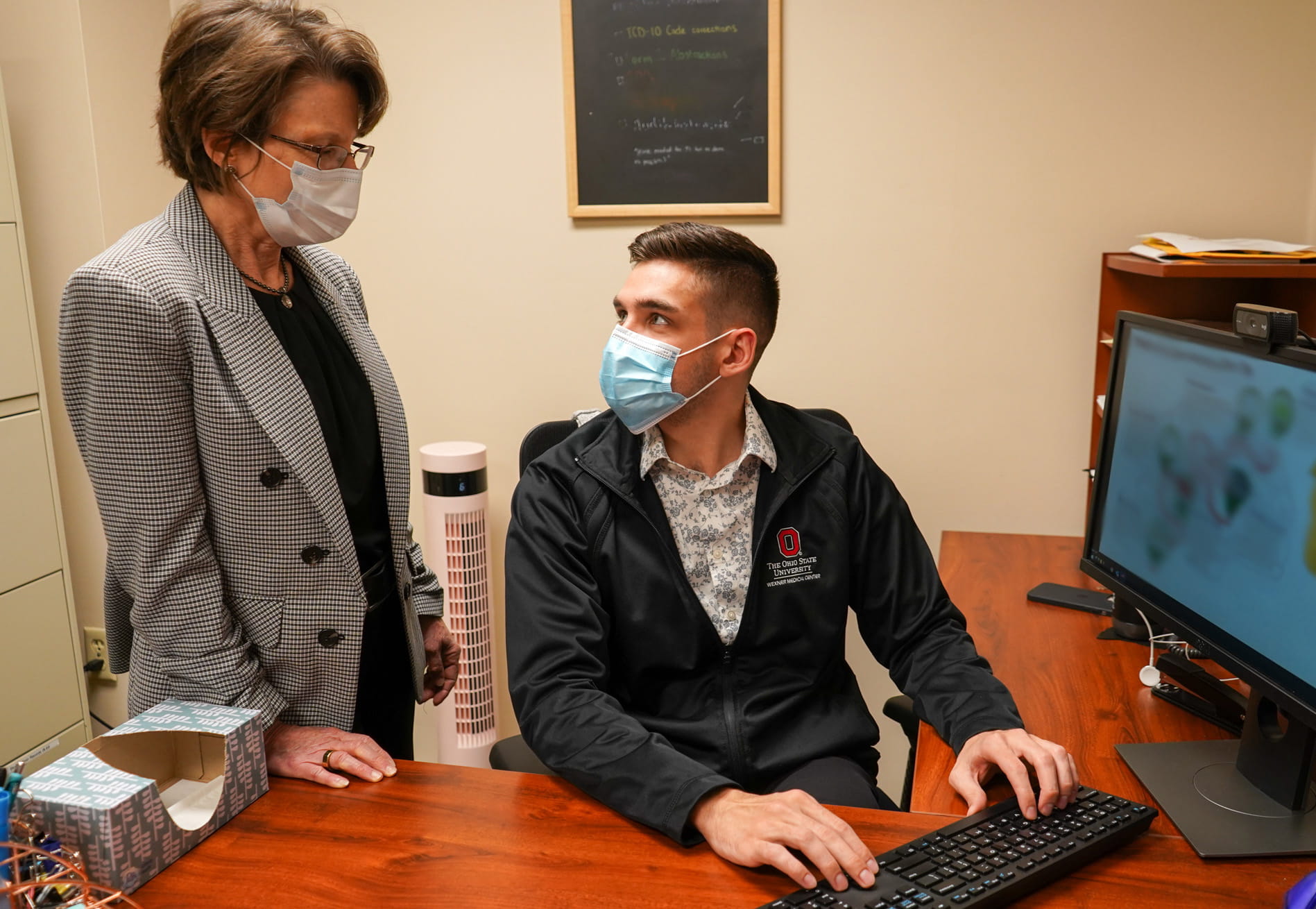 “As we were studying people longer, we began to see that a lot changed for them after five years. We saw some great improvements, but also some declines in many individuals,” said Jennifer Bogner, professor of physical medicine and rehabilitation at Ohio State’s College of Medicine. “Many of the people we speak with have lifelong problems with thinking, problem-solving or behavior regulation. Unfortunately, those struggling with the long-term effects of a TBI are often unsupported after initial treatment, which exacerbates these issues.”
“As we were studying people longer, we began to see that a lot changed for them after five years. We saw some great improvements, but also some declines in many individuals,” said Jennifer Bogner, professor of physical medicine and rehabilitation at Ohio State’s College of Medicine. “Many of the people we speak with have lifelong problems with thinking, problem-solving or behavior regulation. Unfortunately, those struggling with the long-term effects of a TBI are often unsupported after initial treatment, which exacerbates these issues.”The study, funded by the National Institute on Disability, Independent Living, and Rehabilitation Research, checks in with TBI patients annually for two years following their injury and every five years thereafter for the rest of their lives. Phone calls include discussions about their progress and setbacks, as well as common issues for those with TBIs such as mental health disorders and substance abuse. The study revealed that the treatment philosophy for TBI needs to change.
“When we  started to look at these longitudinal outcomes and recognize that stability was not the most common, that change was the most common, we started realizing we need to reconceptualize traumatic brain injury as a chronic condition,” said John Corrigan, director of the Ohio Valley Center for Brain Injury Prevention and Rehabilitation. “Brain injury is more like diabetes or obesity, which is a condition you now have that you’re going to have to actively manage the rest of your life to get your best outcome.”
started to look at these longitudinal outcomes and recognize that stability was not the most common, that change was the most common, we started realizing we need to reconceptualize traumatic brain injury as a chronic condition,” said John Corrigan, director of the Ohio Valley Center for Brain Injury Prevention and Rehabilitation. “Brain injury is more like diabetes or obesity, which is a condition you now have that you’re going to have to actively manage the rest of your life to get your best outcome.”
 started to look at these longitudinal outcomes and recognize that stability was not the most common, that change was the most common, we started realizing we need to reconceptualize traumatic brain injury as a chronic condition,” said John Corrigan, director of the Ohio Valley Center for Brain Injury Prevention and Rehabilitation. “Brain injury is more like diabetes or obesity, which is a condition you now have that you’re going to have to actively manage the rest of your life to get your best outcome.”
started to look at these longitudinal outcomes and recognize that stability was not the most common, that change was the most common, we started realizing we need to reconceptualize traumatic brain injury as a chronic condition,” said John Corrigan, director of the Ohio Valley Center for Brain Injury Prevention and Rehabilitation. “Brain injury is more like diabetes or obesity, which is a condition you now have that you’re going to have to actively manage the rest of your life to get your best outcome.”As researchers learn more about risk factors for decline and variables associated with improvement, they are designing new interventions and protocols to help places like hospitals, homeless and domestic violence shelters, treatment centers and prisons screen for those with TBIs and provide effective care.
“Community resources and service centers need to know if the people they're working with have a history of traumatic brain injury,” said Corrigan, co-principal investigator of the Ohio Regional TBI Model System, which is one of one of 16 federally funded centers in a national network. With funding since 1997, the Ohio center is longest continuously funded site in the network, and its most recent award of $2.26 million provides support through mid-2027.
“A lot of folks with brain injuries are trying to remain in their communities and live independently, and it’s critical that those who can help them do that have a full understanding of how their brain injury affects their actions and abilities so they can provide appropriate accommodations,” Corrigan said.
Some of those accommodations may be as simple as adjusting communication based on a patient’s needs and challenges, which may include reminders about appointments or simplifying messages
or action steps in therapy.
“Some TBI patients may miss appointments simply because they forgot. Or they can’t pay attention in the therapy session because they're having problems following the conversation. But if their treatment provider understands that their traumatic brain injury is causing these problems, then they can make some accommodations,” said Bogner, co-principal investigator of the Ohio Regional TBI Model System.
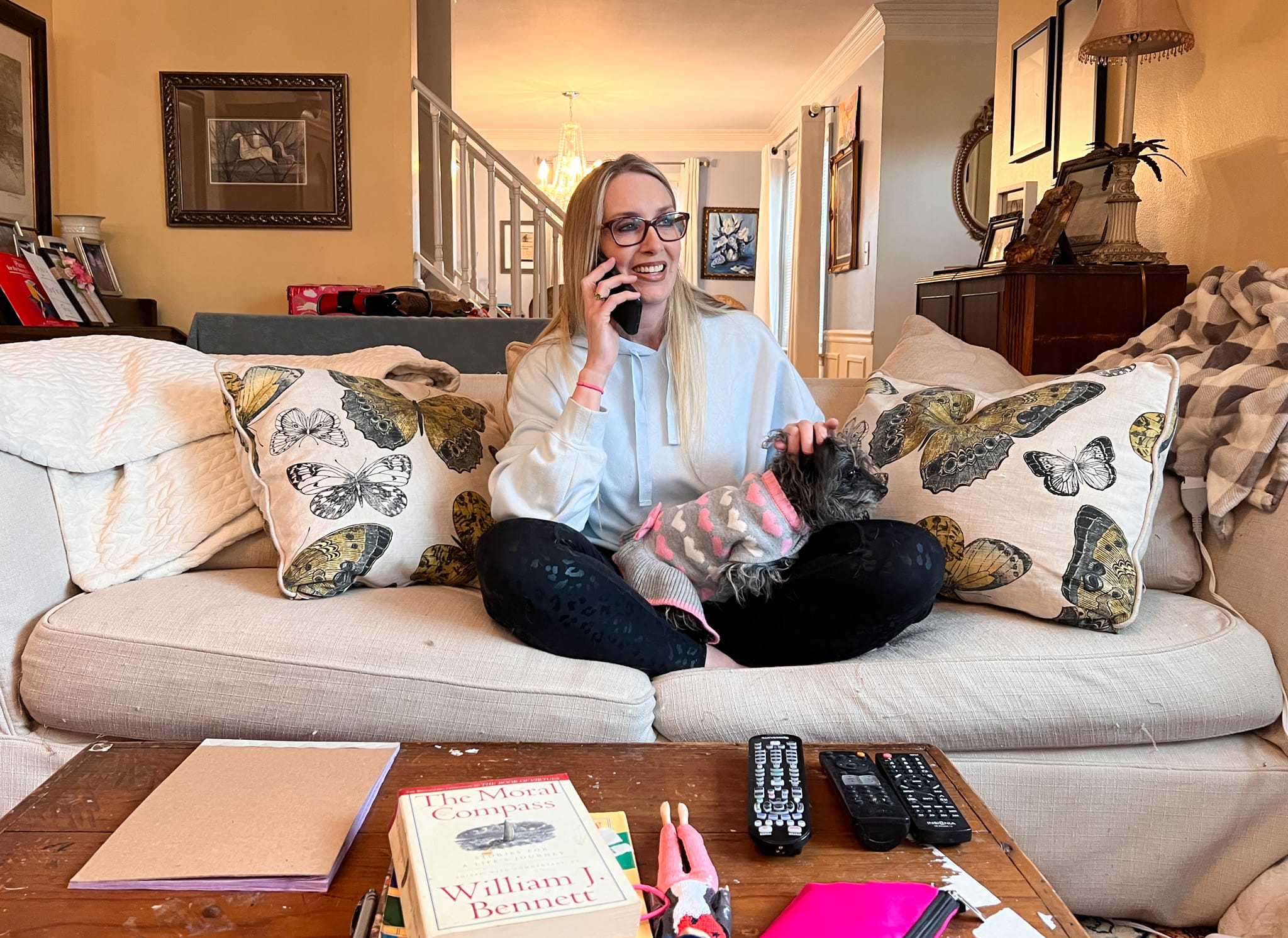 Because researchers conducting the study have long-standing relationships with patients, they’re able to refer them to programs that can help them manage and even improve their condition years after their initial injury. It also helps experts identify gaps in care and needed changes to help improve services and positively impact the lives of those living with the ongoing effects of TBIs.
Because researchers conducting the study have long-standing relationships with patients, they’re able to refer them to programs that can help them manage and even improve their condition years after their initial injury. It also helps experts identify gaps in care and needed changes to help improve services and positively impact the lives of those living with the ongoing effects of TBIs.Corrigan says educating people about TBI can help patients live better lives.
“What we would want, ideally, is not only your initial care is good, but that people understood the lifelong implications, and that your healthcare, social service systems, your family and you all had the education and support you needed to have that optimum life,” Corrigan said.
# # #
Media Contact: Eileen Scahill, Wexner Medical Center, Eileen.Scahill@osumc.edu

