February 1, 2017
 COLUMBUS, Ohio – Unique research being done inside a laboratory at The Ohio State University Wexner Medical Center is changing the way doctors treat one type of irregular heartbeat called atrial fibrillation. Scientists here are the only ones in the world studying revived human atria, donated after a heart transplant, and translating their findings to improve treatment.
COLUMBUS, Ohio – Unique research being done inside a laboratory at The Ohio State University Wexner Medical Center is changing the way doctors treat one type of irregular heartbeat called atrial fibrillation. Scientists here are the only ones in the world studying revived human atria, donated after a heart transplant, and translating their findings to improve treatment.The technique was created by Vadim Fedorov, an associate professor in Ohio State’s Department of Physiology and Cell Biology. Once a donated heart is received, Fedorov’s team has a precious 12 hours to prepare the atria and collect data.
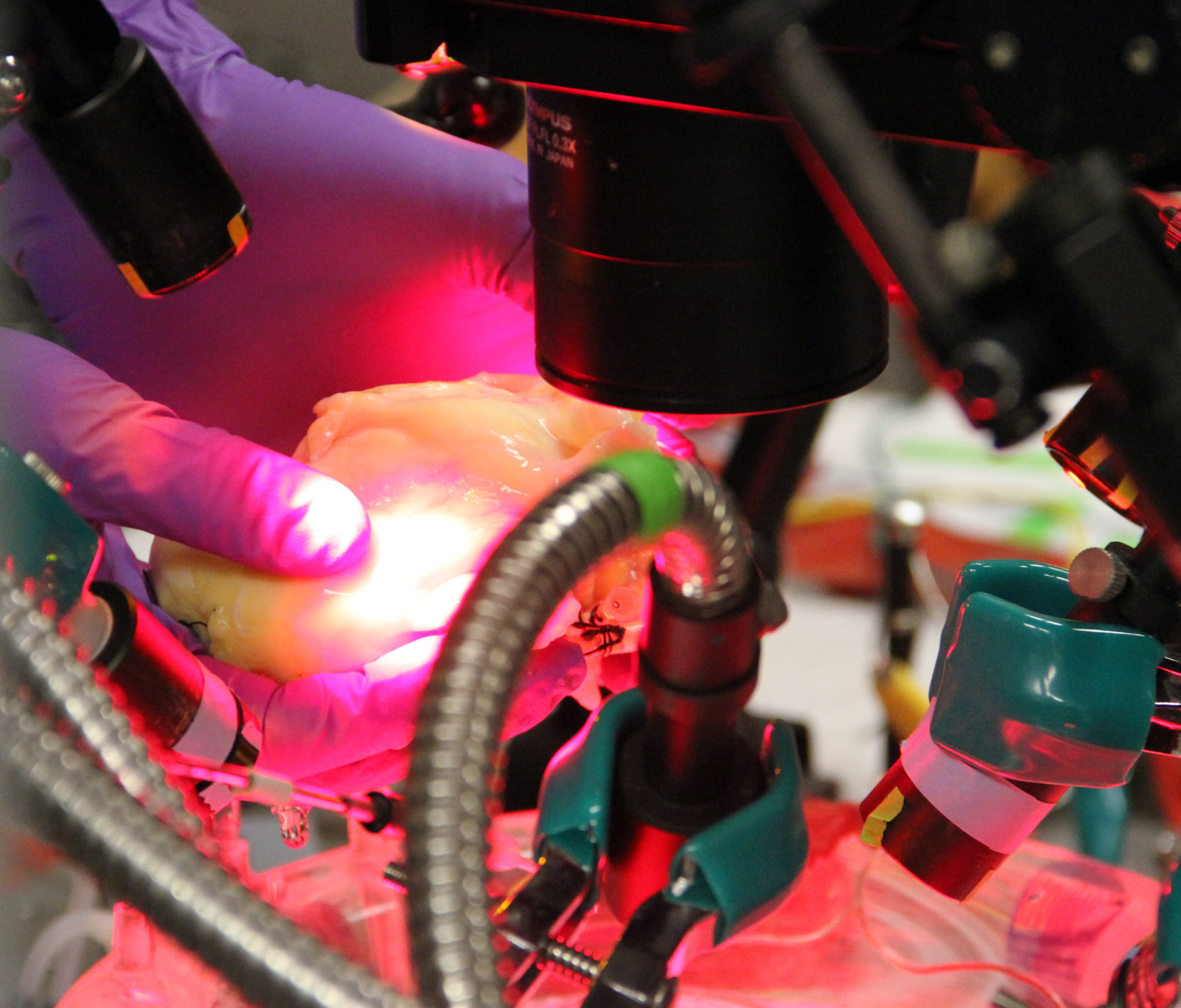
The heart tissue is placed in a dish surrounded by four highly-sensitive infrared cameras, and a fluorescent dye that can sense electrical activity is injected.
“We can see 40,000 recordings across the heart and we can visualize the electrical activity in 3D. We can see through the heart. We can see at many different depths. It’s a vast improvement over any current clinical imaging, where you see up to 200 recordings, and only from one side,” Fedorov said.
 This allows Fedorov and his team to see how electricity spreads across the heart tissue and which areas are responsible. His human heart model confirms what has already been seen in animals – there are regions that look like the eye of a hurricane, called reentrant drivers, which sustain the abnormal electrical activity causing atrial fibrillation, or a-fib.
This allows Fedorov and his team to see how electricity spreads across the heart tissue and which areas are responsible. His human heart model confirms what has already been seen in animals – there are regions that look like the eye of a hurricane, called reentrant drivers, which sustain the abnormal electrical activity causing atrial fibrillation, or a-fib.“Vadim’s made a very important contribution to the study of atrial fibrillation. Not only can we see these regions exist in people, we see what the underlying physiology looks like. These insights are already influencing how a-fib is interpreted and mapped in the clinical setting and it improves our understanding of how and where to administer ablation therapy,” said Dr. John Hummel, an electrophysiologist at Ohio State Wexner Medical Center.
To do an ablation, doctors get a CAT scan or MRI of the heart and create a 3D image in their mapping system. This guides where they create tiny scars on the heart tissue to interrupt the abnormal electrical signals involved in irregular heart rhythms. With current imaging and mapping techniques, there’s still some guesswork involved, and the best treatments only work about 70 percent of the time. Patients often return for additional ablations.
The rate of success is even lower for those with persistent a-fib, which lasts 24 hours a day, for several days at a time.
“There’s been this large school of thought that when you get persistent a-fib, that the degree of the disease is profuse and not fixable. Vadim’s research suggests that might not be true, and so Ohio State is a leading center for taking on clinical trials targeting these regions of abnormal electrical activity,” Hummel said.
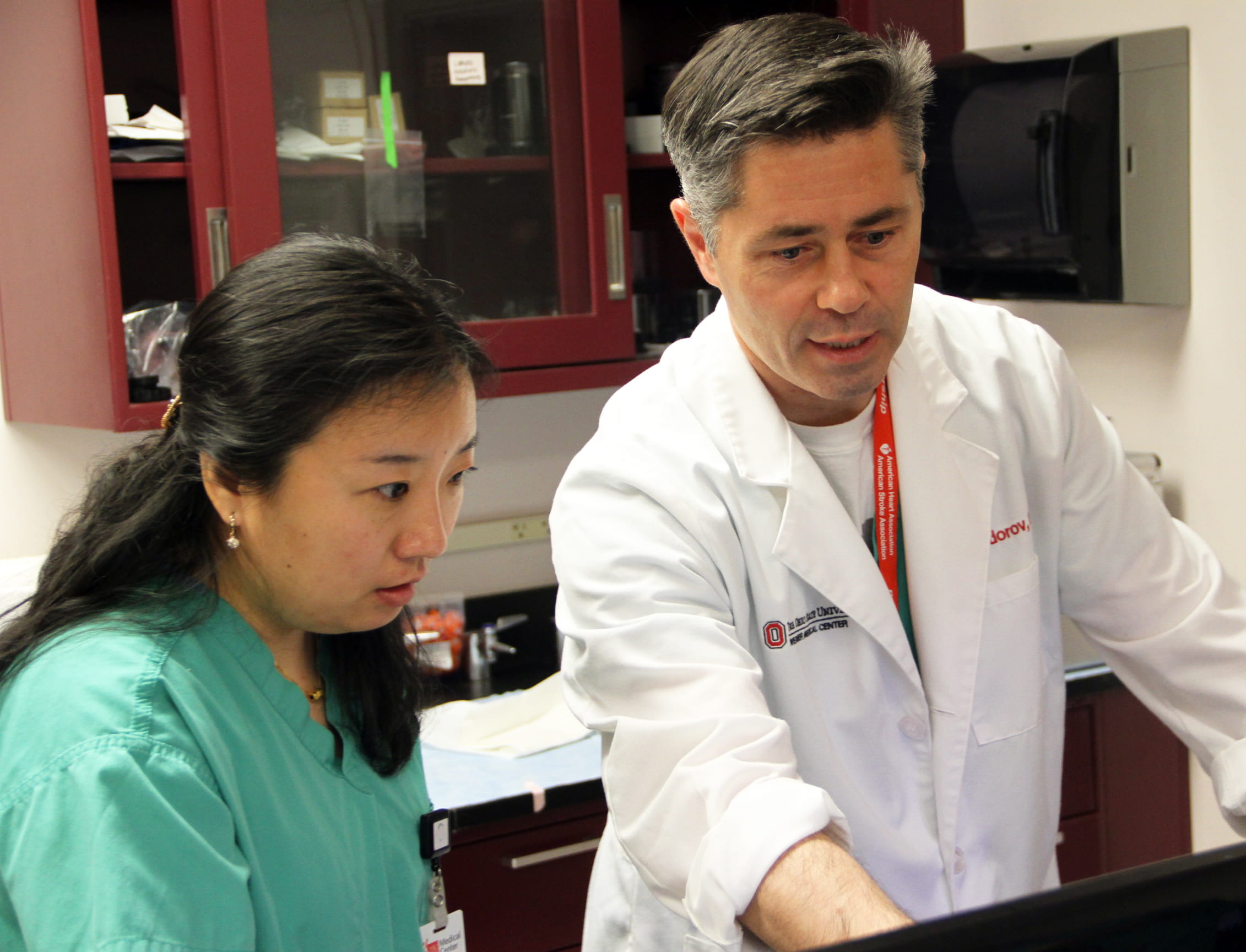
In one study, Fedorov and Hummel are collaborating with Orlando Simonetti and other physician researchers at Ohio State to collect cardiac MRIs and monitor results when patients receive standard ablations. They’re monitoring whether the ablation includes these micro-reentries or not.
“Because we’re not to the point where we can ablate based on the high resolution mapping done in the lab, we’re working it backwards, to verify if the mapping matches where we have successfully ablated,” Hummel said.
This work is crucial because a-fib is the most common type of heart arrhythmia, affecting about six million Americans, he said. When it’s not treated properly, it can lead to blood clots, stroke and heart failure.
“We all talk about the power of translational therapy, but it’s fairly rare that you see such a direct line. This one goes from Vadim’s lab right into our electrophysiology lab. It’s an exciting partnership and I can only imagine what we’d be able to do if we could replicate this level of collaboration at medical centers throughout the U.S.,” Hummel said.
###
Media Contact: Marti Leitch, Ohio State Wexner Medical Center Media Relations
614-293-3737

