April 24, 2017
COLUMBUS, Ohio – A financially strapped pregnant woman’s worries about the arrival and care of her little one could contribute to birth of a smaller, medically vulnerable infant, a new study suggests.
Researchers at The Ohio State University found that pregnancy-specific distress, such as concerns that the baby’s needs won’t be met, appears to be a pathway between financial strain and higher likelihood of a low-birth-weight infant. The study appeared in the journal Archives of Women’s Mental Health.
“There is an opportunity here to look for interventions during pregnancy that could help mitigate the effects of financial strain on birth outcomes,” said lead author Amanda Mitchell, a postdoctoral researcher in Ohio State Wexner Medical Center’s Stress and Health in Pregnancy Research Program.
While larger efforts to improve access to housing, jobs and support for low-income women is critical, there are potential low-cost, stress-reduction techniques that could help reduce risk, Mitchell said. Meditation and breathing exercises could prove useful, for instance, she said.
“It’s important for all women who experience pregnancy-related stress to seek out help coping with that stress,” Mitchell said. “And ob-gyns and other medical providers should also talk about stress during their visits with expecting moms.”
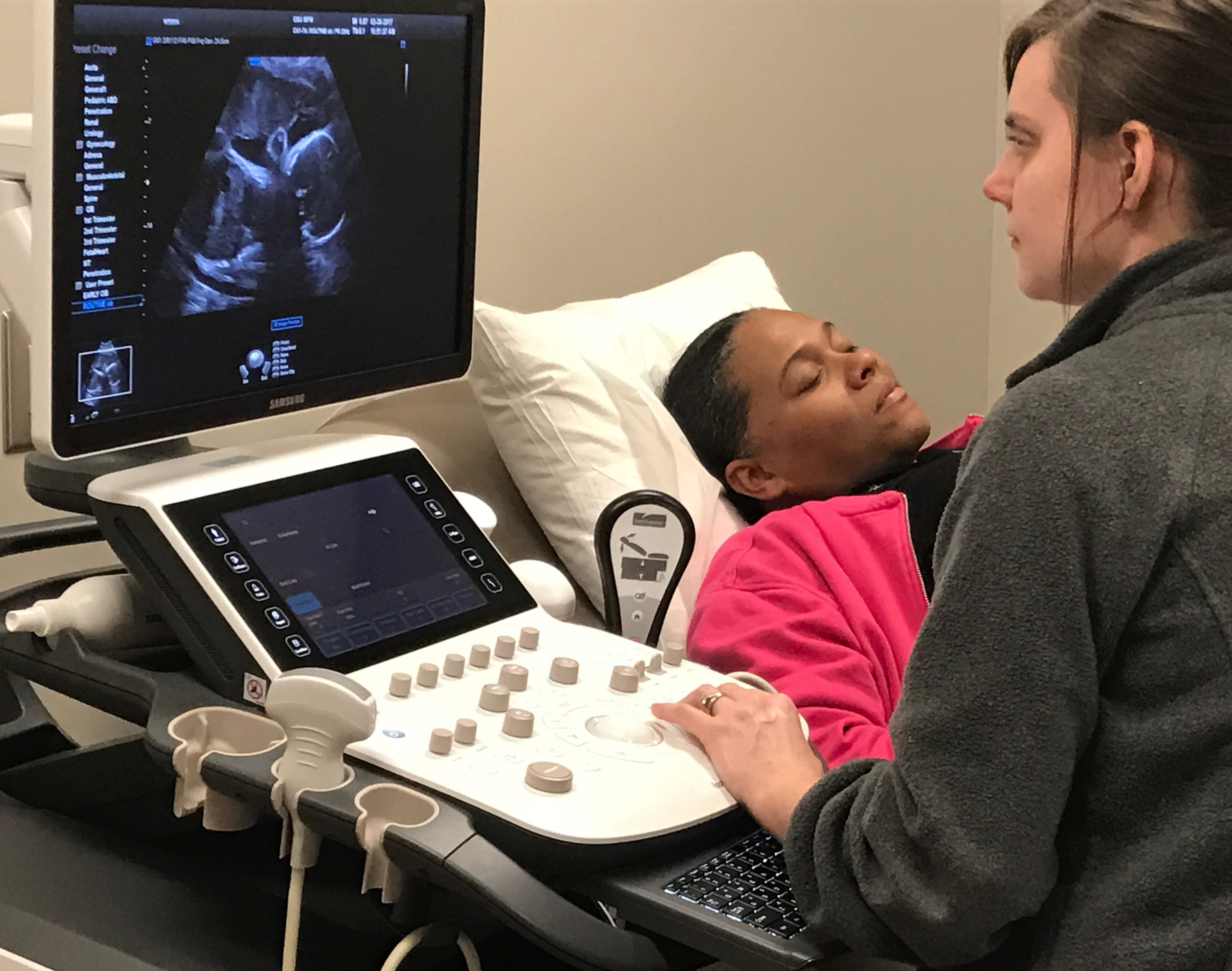 The study included 138 pregnant women who filled out questionnaires to assess financial strain, depressive symptoms, pregnancy-specific distress, perceived stress and general anxiety. Moms in the racially diverse study group were between five and 31 weeks pregnant and 29 years old on average at the time of the assessment. The study, which was primarily designed to evaluate flu vaccine effectiveness, ran from 2013 to 2015.
The study included 138 pregnant women who filled out questionnaires to assess financial strain, depressive symptoms, pregnancy-specific distress, perceived stress and general anxiety. Moms in the racially diverse study group were between five and 31 weeks pregnant and 29 years old on average at the time of the assessment. The study, which was primarily designed to evaluate flu vaccine effectiveness, ran from 2013 to 2015.After the participants’ babies were born, researchers were able to review medical records to compare birth weight against moms’ questionnaire responses during pregnancy.
The researchers knew from previous studies that pregnant moms who are socioeconomically disadvantaged have a higher likelihood of having smaller babies and worse birth outcomes.
What they wanted to learn was whether specific factors could be driving that connection – factors that could lead to positive interventions for women at risk of delivering low-birth-weight babies.
Statistical models designed to identify those drivers landed on one statistically significant factor: pregnancy-specific distress.
“This includes concerns about labor and delivery, about relationships changing, about working after the baby arrives, paying for medical care, and whether the baby will be unhealthy,” said study senior author Lisa Christian, associate professor of psychiatry and a member of the Institute for Behavioral Medicine Research at Ohio State.
Financial strain was assessed based on a five-point scale derived from moms’ responses to three questions: “How difficult is it for you to live on your total household income right now?” “In the next two months, how likely is it that you and your family will experience actual hardships, such as inadequate housing, food, or medical attention?” and “How likely is it that you and your family will have to reduce your standard of living to the bare necessities of life?”
Low-birth-weight babies often suffer from serious health problems and spend their first weeks or months in intensive care. About 8 percent of babies born in the United States are underweight at birth. Low birth weight is clinically defined as below 2,500 grams, or 5 pounds and 8 ounces.
“It’s important to understand the factors that make it more likely for a woman with lower socioeconomic conditions to have a baby at higher risk of complications and death,” Mitchell said.
Limitations of the study include the fact that it was a secondary analysis of data collected during a different study, and that the overall number of low-birth-weight babies was small, at 11. The researchers suggest that replicating this study in a larger group would be beneficial.
The Ohio State researchers are working on another study looking at blood biomarkers that might better explain what biological changes could be at play, including inflammation, Mitchell said.
The study was supported by the National Institutes of Health.
###
Media Contact: Alexis Shaw, Wexner Medical Center Public Affairs and Media Relations, 614-293-3737, Alexis.Shaw2@osumc.edu

