June 20, 2024
COLUMBUS, Ohio – In a new study, neuroscience researchers at The Ohio State University have discovered a special type of human white blood cell that has the potential to regrow nerve fibers.
The study findings, published in the journal Nature Immunology, mark a significant leap forward in medical science.
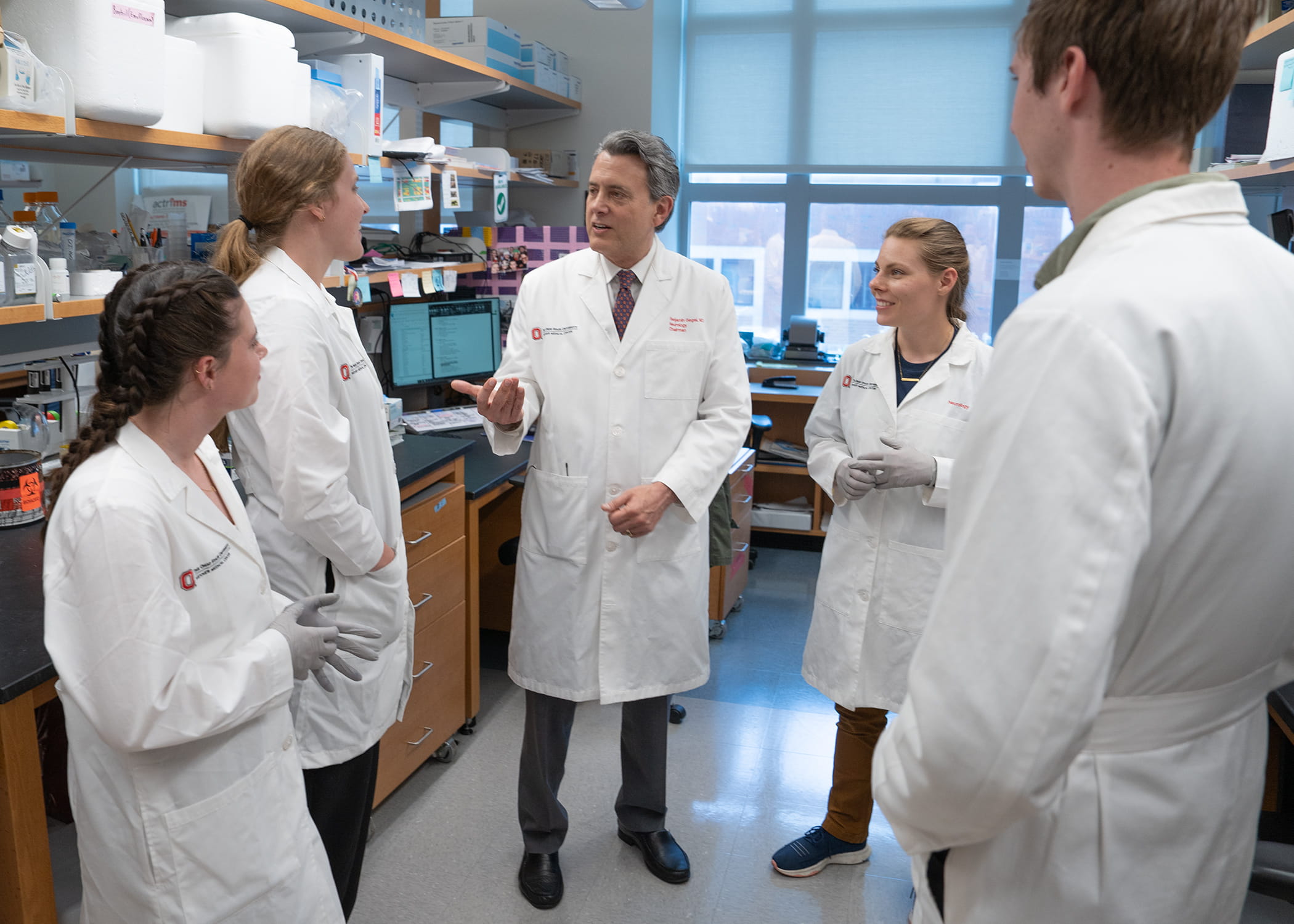
“Dying nerve cells are typically not replaced, and damaged nerve fibers do not normally regrow, leading to permanent neurological disabilities,” said corresponding and senior author Benjamin Segal, MD, professor and chair of the department of neurology at The Ohio State University Wexner Medical Center and College of Medicine.
 Segal's team found that bone marrow cells can be transformed into powerful healing agents. By stimulating these cells with specific molecules in the lab, the team was able to turn them into pro-regenerative cells that can help damaged nerve cells survive and regrow.
Segal's team found that bone marrow cells can be transformed into powerful healing agents. By stimulating these cells with specific molecules in the lab, the team was able to turn them into pro-regenerative cells that can help damaged nerve cells survive and regrow.“Our ultimate goal is to develop treatments using these special cells, to reverse damage in the optic nerve, brain, and spinal cord, thereby restoring lost neurological functions,” said Segal, who is also director of Ohio State’s Neuroscience Research Institute.
Nerve damage from spinal cord, optic nerve or brain injuries, and degenerative neurological diseases such as ALS, Alzheimer’s and multiple sclerosis, has long been believed to be permanent. However, four years ago, Segal's team made a breakthrough in mice, sparking hope for millions affected by these conditions.
“Our new study shows that patients’ own cells can likely be used to deliver safe and effective treatments for these devastating conditions,” said co-first author Andrew Jerome, PhD, a member of Segal’s research team.
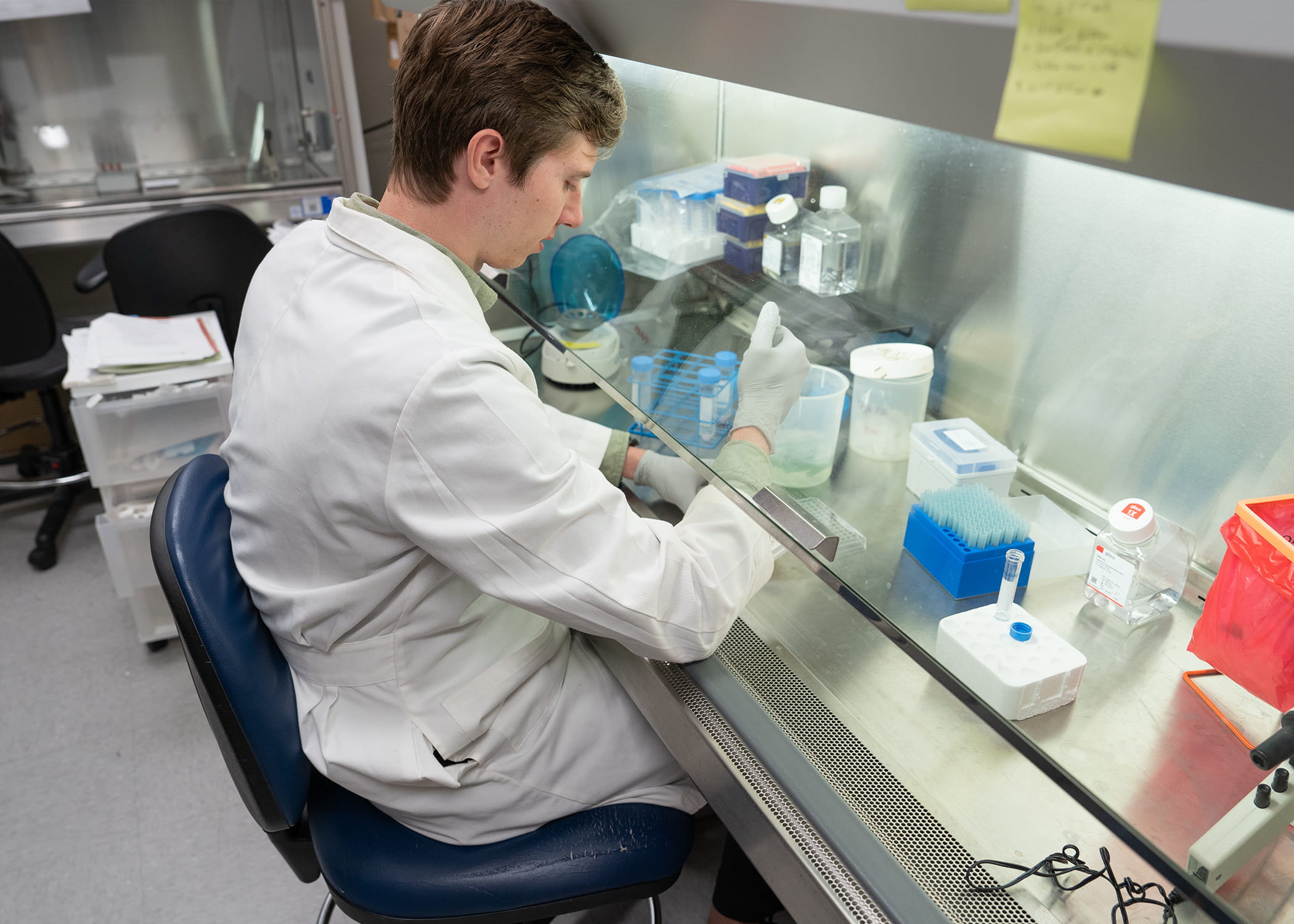 In their recent study, the team generated pro-regenerative cells from the bone marrow of eight different human donors. Remarkably, cells from all eight donors successfully drove human nerve cells to regenerate nerve fibers. These cells even tripled the survival rate of stressed nerve cells. This suggests they can help slow or prevent progression of degenerative neurological conditions, as well as reverse injury and restore function.
In their recent study, the team generated pro-regenerative cells from the bone marrow of eight different human donors. Remarkably, cells from all eight donors successfully drove human nerve cells to regenerate nerve fibers. These cells even tripled the survival rate of stressed nerve cells. This suggests they can help slow or prevent progression of degenerative neurological conditions, as well as reverse injury and restore function. “With the success of these lab experiments, our focus now shifts to bringing these new cell therapy treatments to the patients who need them. We believe these cells can be extracted from a patient, stimulated and grown to large numbers in the lab and reinfused at the site of injury or disease to regrow brain and spinal nerve fibers,” said co-first author Andrew Sas, MD, PhD, assistant professor of neurology at Ohio State.
Segal’s team continues to push these advancements forward. The next steps are to develop the most efficient methods of growing and delivering these cells so clinical trials can begin. Treatments that bring improvements for patients that once seemed impossible are now on the horizon, Segal said.
Media Contact: Eileen Scahill, Wexner Medical Center Medical Relations, Eileen.Scahill@osumc.edu

