From fighting for his life to eyeing triumph in Tokyo
Once the victim of a flesh-eating bacteria, Blake Haxton is now a leader on Team USA in the Paralympics
By all accounts, Blake Haxton shouldn’t even be alive today, much less competing in two different events in the Tokyo 2020 Paralympic Games.
The Ohio State University Wexner Medical Center patient and double-leg amputee will compete in the para-rowing and para-canoeing events in Tokyo.

In March 2009, Haxton went from being a healthy star athlete on the Upper Arlington High School rowing team to a weak and emaciated survivor of an aggressive flesh-eating bacteria that caused a massive blood infection, known as sepsis. Sepsis caused his vital organs, including his heart, lungs and kidneys, to shut down in virtually a matter of hours.
To this day, no one’s really sure how Haxton picked up the bug that cost him both legs – and almost his life.
Initially taken to Riverside Methodist Hospital after complaining of a sore leg after playing in a pick-up basketball game, his condition rapidly deteriorated. While he was in the emergency department, laboratory results and his vital signs indicated sepsis. Physicians also discovered that necrotizing fasciitis, known as flesh-eating bacteria, was causing the pain in his right leg.
Necrotizing fasciitis is a rare but severe and rapidly progressive bacterial infection. It’s associated with significant damage and destruction of deep soft tissue structures, such as the muscle fascia and subcutaneous fat.
To stop the spread of the flesh-eating bacteria, surgeons amputated his right leg above his knee. The sepsis infection worsened in just hours into full-blown septic shock, requiring doctors to place Haxton on a cardiopulmonary bypass machine because his heart and lungs couldn’t keep him alive.
But that was only a temporary solution. This machine could only support him for a few hours.
Brought here to say his goodbyes
Haxton was swiftly transferred to the Ohio State Wexner Medical Center, where he could be kept alive long enough for his older brother to travel back from college to Columbus to say goodbye to him.
“Things were looking grim,” says Dr. Steven Steinberg, one of the Ohio State trauma surgeons who cared for Haxton. Or as Haxton likes to call him, “the quarterback” of his care team.
“We got a telephone call that painted a really bleak picture of this young man. Basically it was, ‘See what you can do.’ So we weren’t expecting too much. I said, ‘Sure.’ When he arrived at Ohio State, he was basically dead. He had no cardiac function. We didn’t know if the infection was curable.”
– Steven Steinberg, MD, professor emeritus
Not out of the woods yet
Because his heart had failed, Haxton was admitted to Ohio State’s Richard M. Ross Heart Hospital, where he was hooked up to an ECMO (Extracorporeal Membrane Oxygenation) machine. ECMO is a type of artificial heart and lung machine that oxygenates a patient’s blood outside the body. At that time, Ohio State was the only local hospital using ECMO to treat patients.
ECMO provides short-term breathing and blood circulation support for patients with cardiopulmonary failure (failing heart, lungs or both). It’s often considered a last-resort option to keep vulnerable patients alive, giving their health care teams extra time to further assess their condition, treat an underlying issue and/or arrange for lung or heart transplantation.
As the medical team at Ohio State treated his severe infection using antibiotics, they noticed that Haxton was starting to improve, ever so slightly.
“By the time his brother had arrived, we could just about turn the ECMO off, and he could survive that. At that point we changed gears. It was still hard for any of us to believe he would survive this,” Steinberg says. “We cautioned the family that he wasn’t out of the woods yet.”
He was still very sick. And his future was anything but certain. Would he survive?
“We kept going and going and going. And he stayed alive,” Steinberg says.
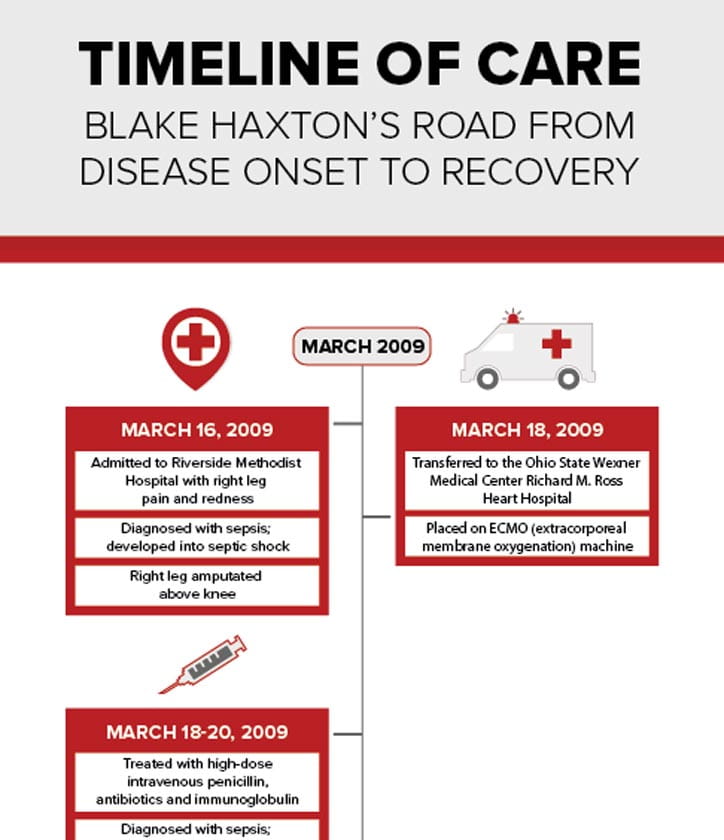
Timeline of care
Blake Haxton's road from disease onset to recovery
Download the full Timeline of Care graphic
Haxton's countless surgeries
Haxton isn’t quite sure how many surgeries he underwent during his month-long stay at the hospital; he lost track around 25, including debridement procedures to remove damaged tissue and skin grafts on both legs and his right arm that also had been affected by flesh-eating bacteria.
A multidisciplinary team of general, orthopedic, vascular and plastic surgeons performed many surgeries focused on trying to save his left leg, which was slowly dying because it wasn’t getting enough blood flow while he was on ECMO. Eventually he lost his left leg at his hip.
During all of this, Haxton was kept in a medically induced coma. He has no recollection of those first six weeks he was hospitalized. He likened it to waking up from a deep sleep, as he slowly regained consciousness.
“I was in a hazy, painful, drug-addled state. I came out very gradually, and when I could finally recognize what was going on, at some level, I knew something was deeply wrong,” says Haxton, who is now 30 and lives in Dublin, where he works as a stock trader at Diamond Hill Capital Management. “But I was grateful to be alive.”

The lucky one
Even now, 13 years later, Steinberg calls Haxton’s recovery “miraculous.”
“If you take 100 patients like Blake, 99 will die. Blake was the lucky one,” Steinberg says.
After eight weeks in the Ross Heart Hospital, on May 13, 2009, he was transferred to the Ohio State Wexner Medical Center’s Dodd Rehabilitation Hospital, where he slowly learned how to navigate his new life using a wheelchair.
“I was in abysmal shape. I was so weak and deconditioned. I didn’t understand how bad things were for me in my recovery,” Haxton recalls. “I didn’t know what to expect. But at that age, time was on my side. I was 18. I had no ongoing complications once the amputations were complete. I was basically fine.”
On June 24, he was discharged to his parents’ home in Upper Arlington, and soon began working with Jennifer Swift, a physical therapist with the Ohio State Wexner Medical Center Outpatient Rehabilitation program.
Haxton had been a star athlete on the Upper Arlington high school rowing team. Being young and healthy had likely helped save his life. But spending 14 weeks in the Ross Heart Hospital and Dodd Rehabilitation Hospital had left him frail and facing a new reality.
Haxton credits Swift with helping him figure out how to tackle his new life without legs. She worked with him for about four months, although he says it took him about two years to fully recover his upper body and core strength.
“She’s another person I can’t say enough good things to say about,” Haxton says with a laugh. “I spent the most time with her during my rehab, and in my case we were working on getting me healthy and building my strength back.”
In addition to overall conditioning, Swift worked with him on how to improve transferring himself in and out of his wheelchair, and in a more advanced move, how to bump up and down the stairs in his wheelchair.
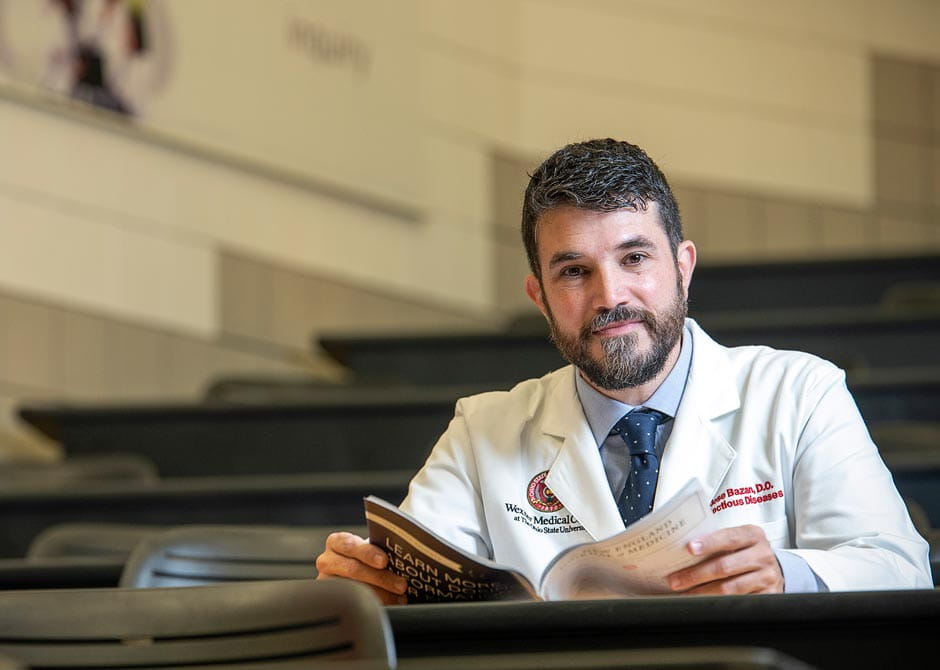
 Left image: José Bazan, DO, infectious disease specialist and member of Blake's original care team.
Left image: José Bazan, DO, infectious disease specialist and member of Blake's original care team.
Right image: Haxton prepares for the 2020 Tokyo Paralympics.
A goal in mind, and a determination to give back
“Blake’s goal was to graduate high school and go to college. He was just go, go, go,” Swift says with a laugh. “He was always motivated and willing to work as hard as he possibly could to do what he wanted to do.”
Swift recalls that he briefly tried and quickly dismissed wheelchair basketball. He missed being active and athletic, but that wasn’t the right sport for him.

“We played a key role in showing him how active he could still be, and as he got stronger, he realized what he could still do,” Swift says. “Blake had the motivation, and we just gave him some direction on what he could try to achieve.”
– Jennifer Swift, physical therapist
2016 Paralympic Games in Rio de Janeiro, Brazil
It was no surprise when she later learned that Haxton had taken up competitive rowing, and that he would be representing the United States at the 2016 Paralympic Games in Rio de Janeiro, Brazil.
While he was training for those games, he attended the first Adapted Sports Conference at Ohio State. In 2017, he was invited to be the keynote speaker at the conference, where he spoke about his personal experience to more than 125 physical, occupational and recreational therapists.
“He talked about how he felt after his amputations, progressing through inpatient and outpatient rehab, to qualifying for the Paralympics. He talked about how therapists can affect and introduce these activities to people as they are going through their recovery process,” Swift says.
Because of the COVID-19 pandemic, the 2020 Paralympics were postponed a year. (Even though the Paralympics are happening in 2021, the event is still referred to by its original year, 2020.)
That delay turned out to be a blessing in disguise for Haxton, allowing him an extra year to train for a new event for him — para-canoeing. But the COVID-19 pandemic remains cause for concern.
“I’m not worried about the disease because I’m young, vaccinated and in good health. I’m worried about catching it and not being able to compete,” he says. “That would be five years of hard work down the drain.”
When he’s not working out on a rowing machine at his home in Dublin, he’s been training six days a week at the Griggs Reservoir on the Scioto River near Upper Arlington.
“I’m from a family of athletes. There’s just something about repetitive low-grade work that is somewhat comforting to me,” Haxton says. “That’s one of the great things about rowing: if you can just be bored and uncomfortable, you’ll probably be pretty good at it.”
He’s considered a “medal threat” in para-rowing after finishing fourth in the men’s single sculls at the 2016 Rio Paralympics. He plans to retire from para-rowing after this year’s Paralympics, but will continue with para-canoeing.
Haxton credits his success to the love of and encouragement from his family and friends, along with his own positive outlook.
“I like to compete. The process of improvement is very incremental – and very slow – but you’re just trying to get a little better every day.”
The Ohio State Wexner Medical Center continues to provide opportunities for athletes like Haxton to achieve their potential in sports through its Adapted Sports Institute, where the team provides athletes with evidence-based and innovative treatment strategies for injury prevention and performance in adapted sports
Haxton has also shared his story in a 2012 Ohio State TEDx talk that focused on the advantages of adversity. And for more than 10 years, Haxton has been invited by Dr. José Bazan to talk to medical students in Ohio State’s College of Medicine about his experiences as a patient. Bazan was part of Haxton’s original care team.
More than 200 medical students gather each January in a large auditorium in Meiling Hall to learn first-hand how the same bacteria that causes strep throat can turn into a life-threatening case of necrotizing fasciitis.
What is necrotizing fasciitis, also known as flesh-eating bacteria?
Explore the frequently asked questions about necrotizing fasciitis, answered by José Bazan, DO.
“What happened was just tragic, but he’s really come out the other end like I would never have imagined. He’s such a humble individual, and for him to give his time year-in and year-out to help train the next generation of physicians is just phenomenal,” says Bazan, an associate professor of Internal Medicine with the Division of Infectious Diseases. “He is just such a good person.”
Haxton enjoys interacting with the students, answering their plethora of questions during and after class. “If there’s something to be learned, something to be gained from my unusual case…I’ve been so fortunate in my recovery,” Haxton says.
While he enjoys sharing his story with medical students, he’s hesitant to visit patients because he understands and respects that each patient’s journey is unique and personal.
But he does have one piece of advice for patients: “Keep grinding every day.”
As he explains, that’s the same advice he’d offer to any able-bodied person, too. But this advice is even more relevant to patients at Dodd Rehabilitation Hospital who likely are learning how to navigate a new normal that may no longer include the use of their arms or legs.
“It’s hard for people around the patient who feel very helpless and want to help. But in reality, most of it is up to the patient,” he says. “What each person wants to happen is the biggest factor in what’s going to happen in their recovery.”