What is ECMO?
Extracorporeal membrane oxygenation (ECMO) — sometimes referred to as extracorporeal life support (ECLS) — is a machine that can function as artificial lungs, heart or both. It works by removing blood from your body to add oxygen in and take carbon dioxide out of the blood, returning it back to your body ready for use. ECMO provides short-term breathing and blood circulation support for patients with heart failure and/or lung failure. This can be a lifesaving measure for our sickest patients, giving our health care team extra time to further assess the condition, treat underlying issues or arrange for lung or heart transplantation.
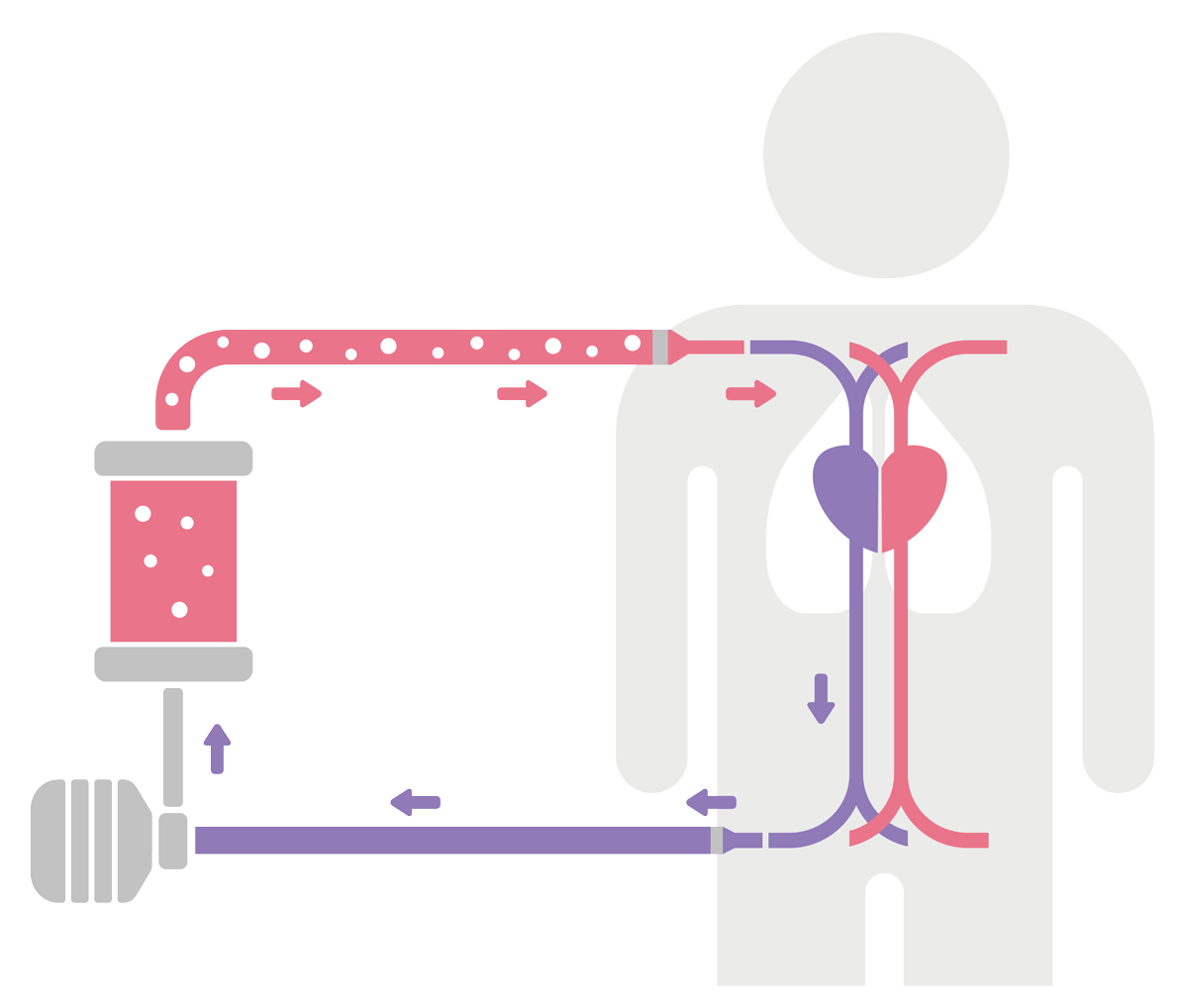
How ECMO works
ECMO replaces the function of your heart and/or lungs in a similar way to how dialysis can take the place of failing kidneys.
Veno-venous (VV) ECMO
This graphic depicts veno-venous (VV) ECMO, which supports the lungs. It uses a unique process of removing carbon dioxide from your blood and then returning oxygenated blood to your body.
A separate type of ECMO is called veno-arterial (VA), which supports both heart and lungs. During VA ECMO, blood is removed from the veins, bypasses the heart and lungs and is then returned back to your arteries — allowing oxygen-rich blood to reach organs.
Most people require ECMO therapy several days to weeks, although some will need to be on ECMO for a longer period of time.
When is ECMO recommended
If you’ve undergone surgery and your care team determines that you need life support so your heart or lungs can heal, you may need to undergo ECMO.
Alternatively, if you need a breathing machine (ventilator) because of lung injury or medications to restore adequate blood circulation because of a failing heart, your specialist may recommend ECMO.

Conditions treated with ECMO
ECMO treats lung and heart diseases such as:
- Bridge to lung or heart transplant
- Bridge to ventricular assist device implantation
- Difficulties recovering from heart surgery
- Severe bacterial or viral pneumonia
- Heart failure
- Lung failure
- Massive heart attack
- Myocarditis
- Postpartum cardiomyopathy
- Pulmonary embolism
- Refractory arrhythmia
What to expect when starting ECMO
Your doctor inserts a thin, flexible tube (cannula) into one of your veins to draw out blood. A second tube that runs into another vein or artery returns warmed, oxygenated blood to your body. You’ll receive sedation medications to help you relax during the procedure. You may not be able to talk while you’re undergoing ECMO. Depending on your situation, you may need to receive ECMO for a few days or up to a few weeks.
Benefits of ECMO
If you’re on a ventilator due to serious health issues, like a respiratory infection, your lungs can become further damaged by the high pressures and levels of oxygen required to support bodily processes. ECMO gives time for your body to recover while allowing the lungs to rest. This provides better outcomes and a better quality of life after you leave the hospital.
Similarly, if your heart is too weak to work and support your tissues with enough blood, an ECMO machine takes over the heart function and circulates the needed blood around your body. During the therapy time, your heart is given a chance to recover or give our medical professionals time to find other solutions to save your life.
ECMO results
How well your body responds to ECMO depends on how severe your condition was prior to starting treatment, as well as other factors. Your doctor and care team will provide details on the results you may expect.
Why choose Ohio State for ECMO treatment?
The Ohio State University Wexner Medical Center is one of a handful of centers in the Midwest that can provide this treatment option to patients who are very sick and experiencing either cardiac or respiratory failure. The Ohio State Wexner Medical Center has extensive experience managing a large number of ECMO patients annually, including the most complicated patients who can’t be managed at other hospitals. For immediate patient care assistance, please have your physician or specialist contact our hospital and ask for the ECMO transfer center.
Our Richard M. Ross Heart Hospital is home to a highly skilled and experienced ECMO team, which includes 24/7 management by our team of cardiac surgeons, critical care doctors and cardiologists. While ECMO offers temporary support, we offer the full spectrum of advanced treatment, including ventricular-assist devices and heart and lung transplantation.
With newer technology, we can transport patients on ECMO from other hospitals. This technology allows our Level I shock program to provide the entire range of advanced therapies to treat patients with acute cardiopulmonary decompensation (deterioration).
Our team is committed to excellence in extracorporeal life support including clinical outcomes, education and research. We also strive to create and grow partnerships with local, state and nationwide hospitals to promote collaboration in ECMO care.
Our leadership team

(Pictured above from left to right: Lauren Kirkland, RN, CCRN-CSC, ECMO Program Manager; Kukbin Choi, MD, ECMO Program Surgical Director; Rafal Kopanczyk, DO, ECMO Program Medical Director; Eric Stallkamp, CCP, ECMO Program Coordinator)

