 When you have a medical condition that makes it difficult to speak, communication challenges can complicate every part of your life, including your ability to get medical care. That’s why augmentative and alternative communication (AAC) is so important. AAC is a set of tools, strategies and technologies that help people express themselves when speech or writing isn’t enough. From picture boards and communication books to high-tech speech-generating devices and apps, it’s important to explore all the options to find the right combination of tools for you.
When you have a medical condition that makes it difficult to speak, communication challenges can complicate every part of your life, including your ability to get medical care. That’s why augmentative and alternative communication (AAC) is so important. AAC is a set of tools, strategies and technologies that help people express themselves when speech or writing isn’t enough. From picture boards and communication books to high-tech speech-generating devices and apps, it’s important to explore all the options to find the right combination of tools for you.
At The Ohio State University Wexner Medical Center’s Assistive Technology Center in Columbus, Ohio, our AAC specialists integrate clinical expertise, research and the latest technology to create personalized communication solutions that enhance independence and quality of life.
What is augmentative and alternative communication?
Augmentative and alternative communication enables children and adults with limited or no speech to express thoughts, needs, wants and ideas. Those with communication impairments use augmentative and alternative communication to supplement or replace speech entirely, depending on each individual.
Types of AAC
At Ohio State’s Assistive Technology Center, AAC tools can be used individually or in combination. Someone who becomes fatigued from speaking verbally throughout the day may use a combination of low- or high-tech AAC tools to communicate their needs and make social connections.
These tools include:
- Picture board communicators
- Text-to-speech options
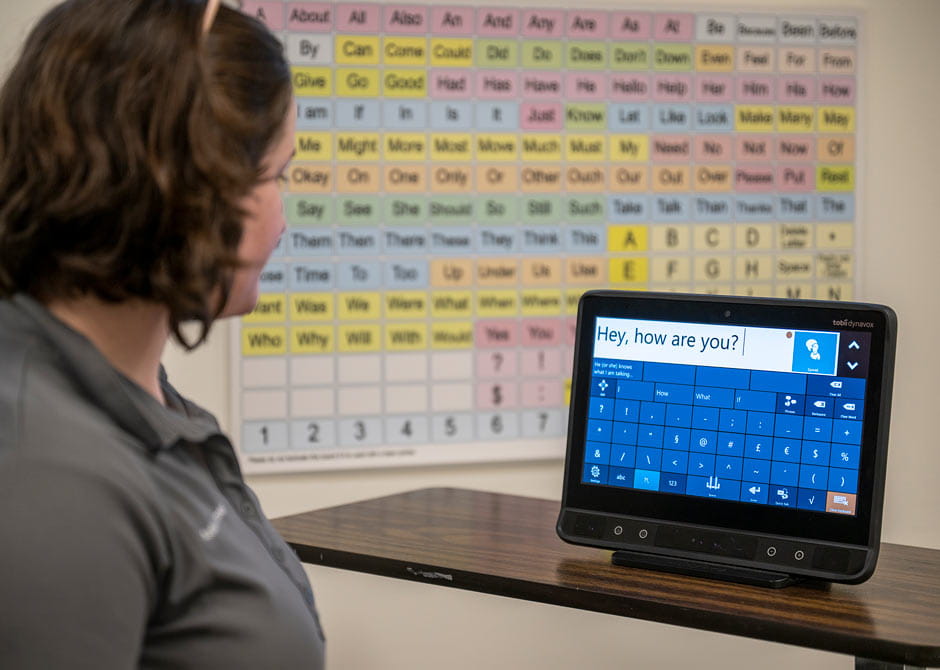
- Speech-generating devices
AAC devices can be personalized to your needs and preferences with wheelchair mounts and unique access methods, such as laser pointers, eye-gaze technology and specially located buttons, or switches. In some cases, voice preservation software can help tailor your device to sound like a digital copy of your natural voice or the voice of a family member, rather than a standard computerized voice.
AAC services offered at Ohio State
Our augmentative and alternative communication program offers therapeutic solutions and access to both low- and high-tech tools. Low-tech AAC includes dry-erase boards, picture-based communication books and similar tools. High-tech AAC includes tablets, speech-generating devices and specialized software.
From evaluation through equipment fitting, training and functional use, the AAC team provides a customized approach to determine the best solution for each person.
Who is a candidate for augmentative and alternative communication?
Some people we care for have never had the ability to communicate verbally, some have communication abilities that are deteriorating because of progressive disorders, and some people have lost the ability to communicate via speech because of a brain injury, stroke or other event.
Referrals to Ohio State’s Augmentative and Alternative Communication Program include individuals who have been diagnosed with:
- Cerebral palsy
- Autism
- Head and neck cancer
- Intellectual disabilities
- Brain injuries
- Stroke
- Voice disorders, such as aphonia
- Speech aphasia and apraxia
- Progressive neurological impairments, such as amyotrophic lateral sclerosis (ALS), Parkinson’s disease, multiple sclerosis and Huntington’s disease
How do I get an appointment for an evaluation with augmentative and alternative communication services at the Ohio State Wexner Medical Center?
Your physician or speech therapist can help you determine whether it’s the right time to seek AAC solutions. A physician can refer you for an evaluation with Ohio State’s AAC services by faxing this information to 614-293-9002:
- Primary medical diagnosis and speech disorder
- A referral for speech therapy
- Statement that AAC is medically necessary for treatment of the individual’s speech disorder
- Most recent office notes
- Medication list
Referring physicians don’t need to be a specific type of doctor or specialist, but they do need to be able to sign off on necessary equipment for insurance purposes.
What’s involved in an evaluation to find the best communication tools for me?
Our AAC specialists use in-depth interviews and dynamic assessments to understand any physical, sensory, cognitive or linguistic challenges you may have, as well as how independently you’re able to communicate verbally.
Our assessment, customization and training process includes the following:
- Comprehensive assessment: At your initial appointment, we’ll evaluate your speech, language, motor and cognitive skills, as well as vision and hearing. Our team will provide more information about augmentative and alternative communication tools, and which devices might be most effective for your unique circumstances.
- Device trials and customization: Following the evaluation appointment, a speech-language pathologist will work with you to decide what types of tools may be best. You’ll have the opportunity to try different systems before selecting one or a combination of tools. Our speech-language pathologists tailor vocabulary and settings to reflect each person’s daily routines and preferences.
- Training and ongoing support: We’ll schedule follow-up appointments to demonstrate the devices, let you test multiple types of equipment and train you on how to use them. We also provide hands-on training for families and caregivers to ensure effective use of AAC devices at home, school or work. As your needs change, follow-up sessions will help refine and expand communication abilities.
How much independence can I expect to gain with my new augmentative and alternative communication tools?
Each person’s level of independence varies based on what tools they’re willing to use, the type of disorder or physical challenges they may have and what their everyday life looks like. The tools we match people with can provide independence beyond just communication. For example, they can help people change the channel on their TV or turn on lights and fans. Many people use their AAC devices to help them gain and maintain employment. Use of a wide range of tools can help reduce the burden of care both inside and outside the home.
Why choose Ohio State for augmentative and alternative communication services?
The augmentative and alternative communication team at the Ohio State Wexner Medical Center is led by a speech-language pathologist who collaborates with other assistive technology providers, such as occupational therapists, physical therapists and rehabilitation engineers, to meet every individual’s communication needs, including needs that change over time.
The AAC clinic is part of the medical center’s Assistive Technology Center and is also certified through the Rehabilitation Engineering and Assistive Technology Society of North America.