What is COVID-19?
COVID-19 is an illness caused by the SARS-CoV-2 virus. Symptoms can include fever or chills, fatigue and body aches, sore throat, headache, cough and shortness of breath. In severe cases, COVID-19 can be deadly.
SARS-CoV-2 that causes COVID-19 was first found in 2019, hence the name COVID-19 for the virus that was at the center of the 2020 pandemic; it was a new (novel) strain of the coronavirus. Previously discovered coronavirus strains included severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS).
How does COVID-19 spread?
COVID-19 travels in respiratory droplets released into the air when an infected person coughs, sneezes, speaks or breathes. You may get infected if you are close by and inhale these droplets.
You can also get it from close contact (touching, shaking hands) with an infected person and then touching your face.
The best ways to prevent catching COVID-19 include staying up to date on COVID-19 vaccines, wearing a mask, practicing social distancing (staying a few feet apart from other people), washing hands and avoiding people who are sick.
Don’t delay — get vaccinated against COVID-19
COVID-19 symptoms
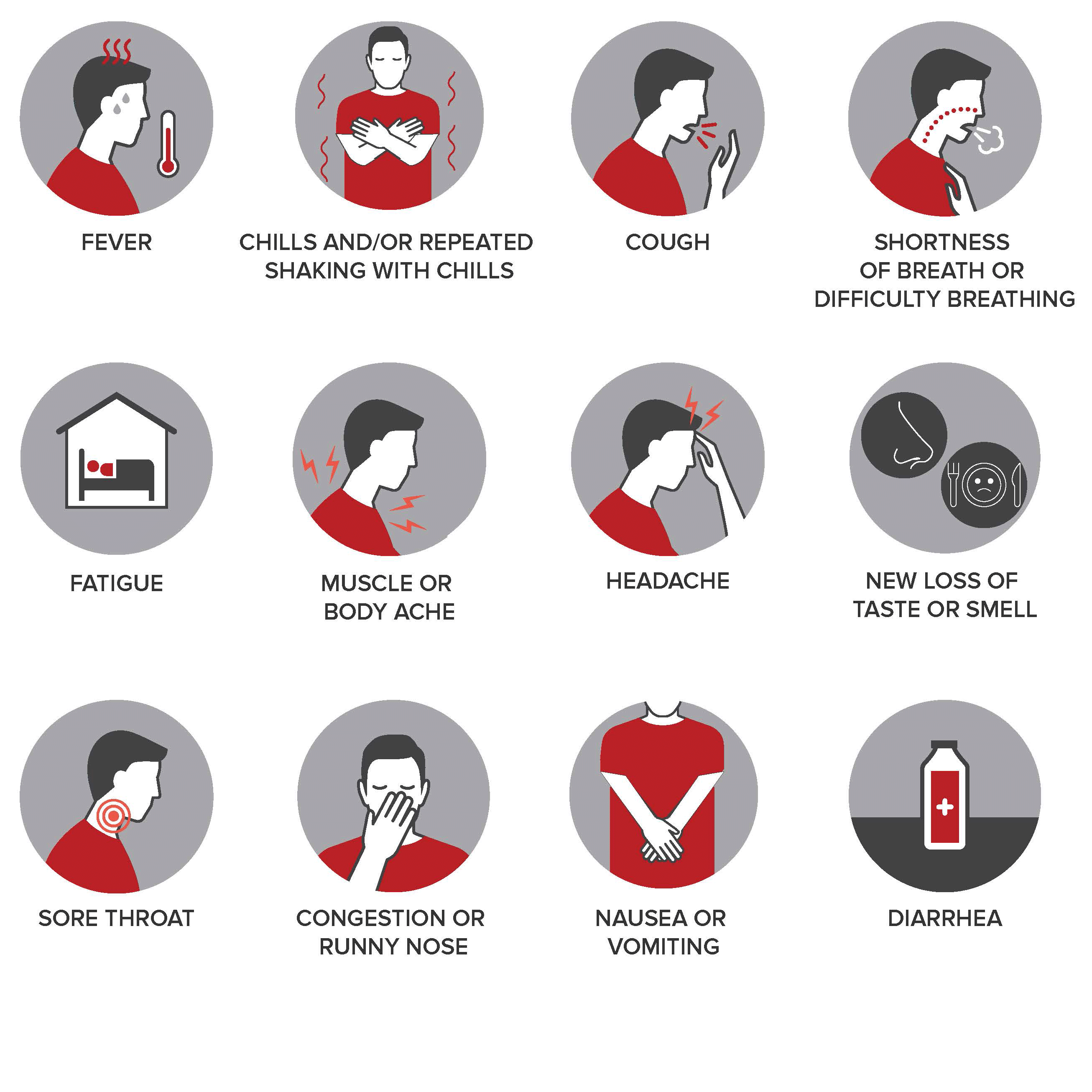
Symptoms may appear 2 - 14 days after exposure. If you have COVID-19, you may have these symptoms:
- Fever
- Chills/shaking chills
- Respiratory symptoms, such as cough or shortness of breath
- Fatigue
- Body or muscle aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Care Companion Program
This service has an interactive, individualized care plan available with MyChart.

Go to the hospital immediately if you’re experiencing:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- Bluish lips or face
