Are headaches a sign of something wrong?
 For millions of people, headaches are a common, generally harmless condition. Very often, headaches indicate stress, lack of sleep or dehydration. However, when a headache becomes particularly persistent or painful, it could reflect a serious, underlying health problem that requires attention.
For millions of people, headaches are a common, generally harmless condition. Very often, headaches indicate stress, lack of sleep or dehydration. However, when a headache becomes particularly persistent or painful, it could reflect a serious, underlying health problem that requires attention.
At The Ohio State University Wexner Medical Center, our team of doctors and specialists know that headache management requires a personalized approach. Whether you’re suffering from cluster headaches or vestibular migraine symptoms, we work with people every day who, just like you, want a path to long-term relief.
Unlike with a bruise or a broken bone, you can’t prove that you’re experiencing a headache, let alone its severity. This is one reason headaches can be so complex to treat.
When should you see a neurologist or headache specialist?
If you routinely go to an urgent care or Emergency Department to manage your headaches or if you’ve tried multiple treatments without success, you should get referred to an Ohio State headache specialist. Call our office today to get started.
Is your facial pain part of a headache issue?
It’s possible the facial pain you’re experiencing is part of a headache disorder. Whether your facial pain is part of an underlying issue, headache disorder or something else, our team is committed to properly diagnosing your condition.
How are headaches treated?
Treating a headache is generally a combination of several different medical approaches, including at-home remedies, medication, lifestyle changes and, in some cases, surgical procedures.
What are at-home remedies for headaches?
You may be able to find headache relief from a bath or shower, essential oils, taking a nap or applying a hot or cold pack to the affected area. A gentle massage to the shoulders or the back of the neck can help too.
Also, at the first sign of a headache, drink a large amount of water.
Stopping headache pain with rescue medication
Medications used to stop headaches or migraine attacks are called acute, abortive or rescue medications. These medications are designed to stop symptoms and are available both over the counter and by prescription.
You may be familiar with over-the-counter medicines like acetaminophen (Tylenol), ibuprofen (Advil or Motrin), naproxen (Aleve) and Excedrin (a blend of acetaminophen, aspirin and caffeine). These shouldn’t be taken for more than two to three days per week. If taken more frequently, you could develop rebound headaches.
Preventing headaches from starting
Preventive medications seek to stop headaches before they start. Your doctor can prescribe beta-blockers, calcium channel blockers, tricyclic antidepressants and calcitonin gene-related peptide (CGRP) inhibitors.
Lifestyle changes to help you avoid headaches
These lifestyle or behavioral changes may help you avoid headaches or lessen the symptoms that do occur:
- Staying hydrated
- Reducing stress with meditation, breathing exercises or other techniques
- Exercising regularly
Botox for headache treatment
On occasion, persistent facial or neck pain might be the main driver of a headache. Your facial or neck pain could be due to irritated nerves. These nerves can be targeted with local injections called “blocks.” If you have more than 15 headache or migraine days per month, Botox injections in the face, neck, and shoulders could help reduce your symptoms.
Surgical treatment of headaches
If other medications or treatments have failed to give you relief from headaches or migraine attacks, or if the underlying condition is abnormal or very serious, your doctor may recommend nerve decompression surgery. This procedure eases constriction of nerves that can cause your symptoms.
What causes a headache?
 Headaches can be caused by tension in the neck and head muscles, changes in blood flow to the brain or by activation of pain-sensitive areas in the head. Alternatively, underlying conditions such as migraines attacks, sinus infections or dehydration can cause headaches.
Headaches can be caused by tension in the neck and head muscles, changes in blood flow to the brain or by activation of pain-sensitive areas in the head. Alternatively, underlying conditions such as migraines attacks, sinus infections or dehydration can cause headaches.
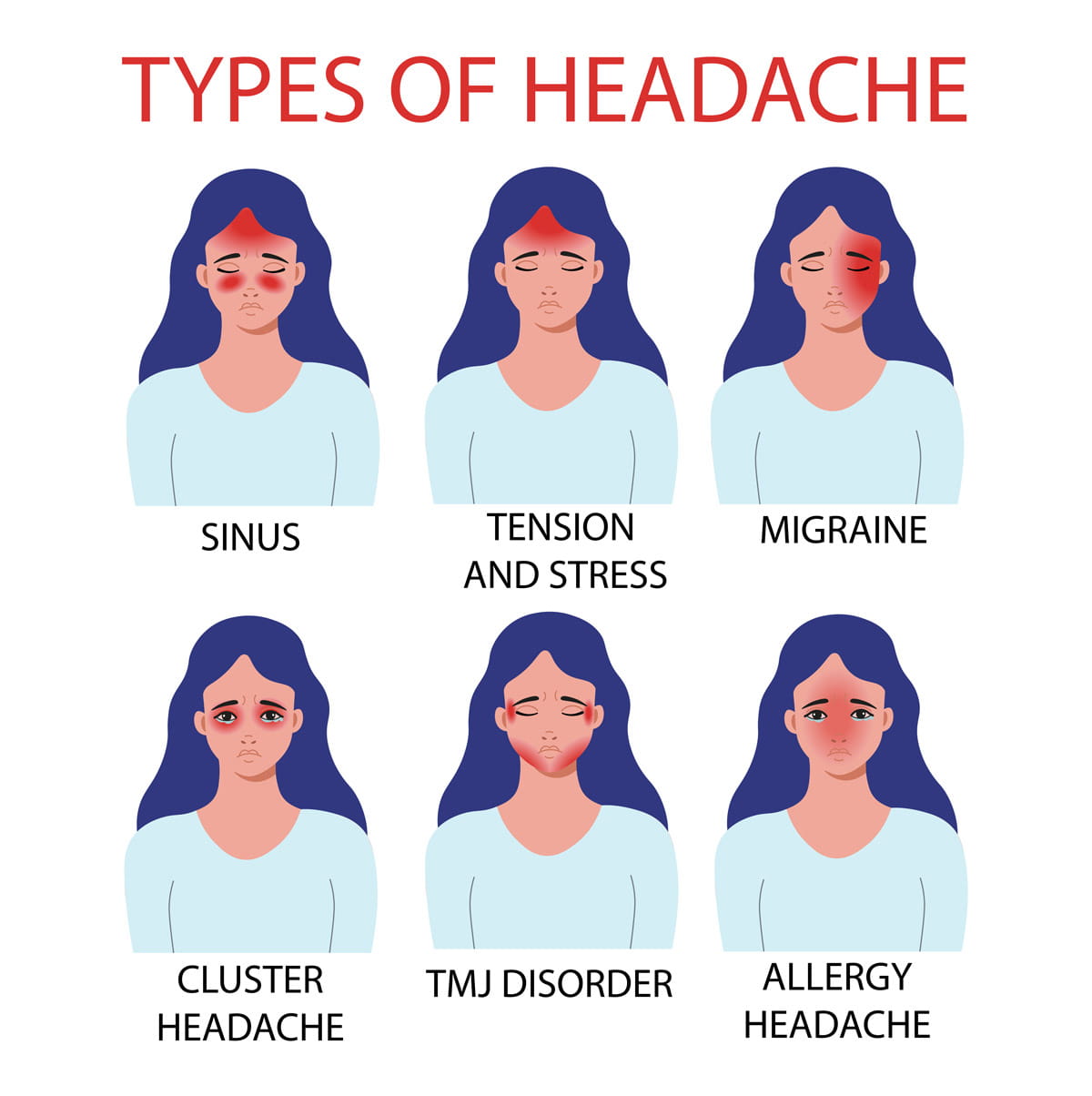
Headaches are categorized as either primary or secondary, based on their root cause.
Primary headaches
Primary headaches are standalone conditions that include tension-type headaches, ocular headaches, cluster headaches and migraine.
Migraine
Arguably the most well-known type of headache, migraine is also one of the most commonly misunderstood. For example, it isn’t just “a bad headache.” Migraine is a debilitating neurological disorder that seriously impacts the lives of millions of people.
While symptoms vary from person to person, a migraine onset typically causes severe throbbing or pulsating pain on only one side of the head. Migraine episodes are also associated with a heightened sensitivity to light, sound and smell, as well as nausea and vomiting.
Tension headaches
Tension headaches are very common and typically moderate in their intensity. Usually related to stress and muscle tension, tension headaches may include band-like pressure around the head.
Primary cough headaches
Primary cough headaches are brief and intense, which can be triggered by coughing, sneezing or straining. While largely harmless, these can be recurrent and sometimes require medical attention.
Other types of primary headaches
- Chronic headaches are characterized by headaches 15 or more days per month for at least three consecutive months.
- Cluster headaches, known for their intense stabbing pain and recurring frequency, are rare. Symptoms often include severe pain in only one side of the head, a runny nose or watering eyes.
- New daily persistent headache is a condition where you experience persistent and continual headaches, often coming on suddenly with no clear cause.
- Primary exertion headaches happen during or after intense physical activity and are possibly related to changes in blood pressure or flow.
- Primary stabbing headaches are sudden, sharp and short-lived. Sometimes called “ice pick headaches,” because of how intense the pain is to those who experience it.
- Vestibular migraine is a neurological syndrome that causes balance problems. In addition to intense migraine pain, vestibular migraine symptoms tend to also include dizziness, lightheadedness, nausea and vertigo. In some cases, vestibular migraine symptoms don’t cause headache symptoms at all.
Secondary headaches
Secondary headaches cause symptoms from an underlying medical problem that needs treatment. By addressing the underlying condition, your headache symptoms should lessen or go away entirely. Infections, head injuries, sinus problems, high blood pressure and vascular disorders are the most common reasons for secondary headaches.
Concussion headaches
Concussion headaches are a common symptom of a concussion, which is a traumatic brain injury resulting from a blow or jolt to the head. We work closely with the experts at Ohio State Sports Medicine to treat concussions that occur during sports or athletic activities.
Our team of headache specialists routinely treats complex concussions.
Other types of secondary headaches
- Headaches in children can be challenging to identify and treat. Causes may include allergies, dehydration, dental issues, eye problems or illness.
- Hormone headaches are caused by changes in hormonal levels (particularly during menstruation, pregnancy or menopause). Symptoms include a dull throbbing sensation in the head and neck, fatigue, dizziness and sensitivity to sounds and light.
- Low cerebrospinal fluid (CSF) headaches happen because of a spinal fluid leak, which is often caused by a spinal tap, recent spinal surgery or head and neck trauma. Typically, these types of headaches begin shortly after you stand up and tend to go away when you lie down. CSF pressure-related headache pain is typically worse near the back of the skull.
- Rebound headaches (formerly known as “medication overuse” headaches) are both painful and preventable. These can occur if you use too many pain relievers or anti-migraine medications to get rid of a headache, which only tends to worsen the situation. The original headache pain will return (or “rebound”) with even more intensity.
- Sinus headaches are relatively rare. In fact, most “sinus headaches" tend to be misdiagnosed migraine symptoms, or tension headaches with sinus-related symptoms.
- Thunderclap headaches are intense, sudden-onset headaches that reach a maximum severity within 60 seconds. These often suggest a serious underlying medical condition requiring immediate attention.
How are headaches diagnosed?
To properly diagnose and treat your headache symptoms, we use a variety of diagnostic tools (such as imaging studies and blood tests) to find the cause.
Our headache specialists will work closely with you to learn more about your symptoms and identify the specific kind of headache that you’re experiencing.
Why choose Ohio State for headache treatment?
Ohio State continues to pioneer technologies and therapies related to headache and migraine care. At the Ohio State Headache Center, you’ll receive care from a multidisciplinary team of nationally ranked experts. Multidisciplinary care means we often work with our colleagues in neuromodulation, plastic surgery and interventional pain management. We’re a team that’s committed to you for the long haul.
For headache treatment at Ohio State, you may also be seen by our expert physical therapists, headache clinical pharmacist and integrative medicine specialists (offering chiropractic services, acupuncture, massage, etc.). Plus, we have a network of infusion centers for acute treatment of migraine, as well as for preventive medication.


