 What is discitis?
What is discitis?
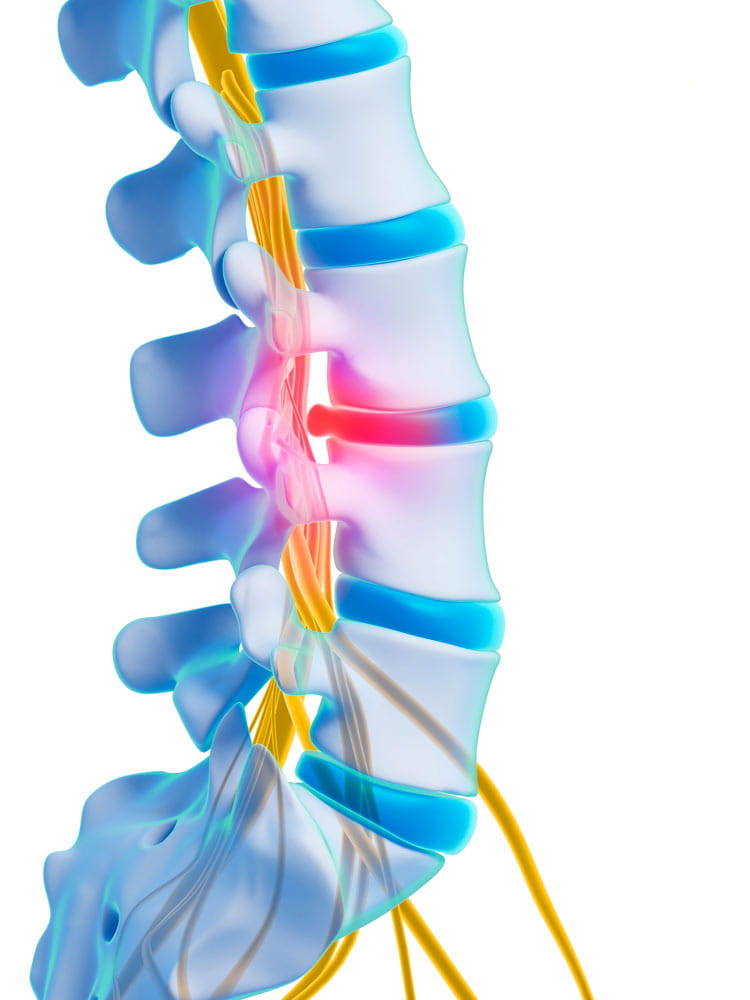
Discitis is a serious but uncommon condition characterized by inflammation of the intervertebral discs, which are the soft, cushion-like structures located between the vertebrae of the spine. This inflammation is mostly commonly caused by an infection, usually bacterial, although it can also result from other factors, such as trauma or autoimmune disorders.
Discitis can lead to pain and discomfort in the affected area of the spine, typically in the lower back or neck, which may worsen with movement or pressure on the spine. Other symptoms may include stiffness, swelling and tenderness in the affected area, as well as fever and chills if the inflammation is due to an infection.
What are the symptoms of discitis?
Symptoms of discitis can vary depending on its severity, although common signs and symptoms include:
- Persistent, localized back pain, usually in the lower back or neck
- Pain that worsens with movement or activity
- Tenderness and swelling in the affected area of the spine
- Stiffness and limited range of motion in the spine
- Fever and chills, especially if the inflammation is caused by an infection
- Loss of appetite and fatigue
- Neurological symptoms such as weakness, numbness or tingling in the arms or legs (less common)
How is discitis diagnosed?
Discitis is typically diagnosed through a combination of medical history, physical examination and imaging tests. Your doctor will:
- Gather information: First, your doctor will discuss your medical history with you and work to understand the nature and severity of your symptoms.
- Physical examination: Your doctor will conduct a physical exam to assess your spine’s range of motion, strength of muscles along the spine, reflexes and sensation.
- Blood tests: Blood tests may be done to check for signs of infection, such as an elevated white blood cell count or erythrocyte sedimentation rate (ESR).
- Imaging tests:
- X-rays: These can show changes in the bones and alignment of the spine, such as narrowing of the disc space, bone erosion or abnormal bone growth.
- MRI (magnetic resonance imaging): This provides detailed images of the spine, including soft tissues like discs, ligaments and nerves, allowing the doctor to visualize any inflammation or infection in the disc.
- CT scan (computed tomography): Sometimes used to provide additional detail, especially if MRI is not feasible or is inconclusive.
- Biopsy: In some cases, a sample of tissue from the affected disc may be taken and analyzed to confirm the presence of infection and identify the specific bacteria causing the discitis.
By combining information from these tests, we can accurately diagnose discitis and develop an appropriate treatment plan. Also, if your issue is caused by an autoimmune disorder, we treat the disorder first before anything else.
What is the treatment for discitis?
The treatment for discitis typically depends on its underlying cause and severity. If our experts recommend multiple types of treatments, we may have you stay at the hospital to deliver you the best care possible:
- Antibiotics: If the discitis is caused by a bacterial infection, we’ll prescribe antibiotics to treat the infection. The specific antibiotic and duration of treatment depends on the type of bacteria involved and your overall health.
- Pain management: Pain relief is an important element of your treatment plan. Over the counter or prescription pain medications may alleviate discomfort and improve your mobility.
- Immobilization: Rest and immobilization of the spine may help reduce stress on the affected disc and promote healing. Our team may recommend wearing a back brace or limiting activities that aggravate symptoms.
- Physical therapy: Once the acute phase of the infection has resolved, physical therapy can improve spinal strength, flexibility and posture. Our physical therapists can design a customized exercise program to address your specific needs.
- Surgery: In severe cases, or when conservative treatments fail to provide relief, surgery may be necessary to remove infected tissue, drain abscesses or stabilize the spine.
Who is at risk of developing discitis?
Because discitis is usually caused by an infection, if you’re at higher risk for an infection you also have an increased chance of developing discitis. Specifically, if you have one of the following situations you may have an increased risk:
- Are a child under the age of 10
- Are recovering from surgery (especially of the spine)
- Have an autoimmune disorder
- Have a weakened immune system
- Use intravenous drugs
- Have a chronic medical condition such as diabetes
- Had a recent spine injection therapy
Spinal Stenosis
How would you like to schedule?
Don’t have MyChart? Create an account
