 What is facet joint syndrome?
What is facet joint syndrome?
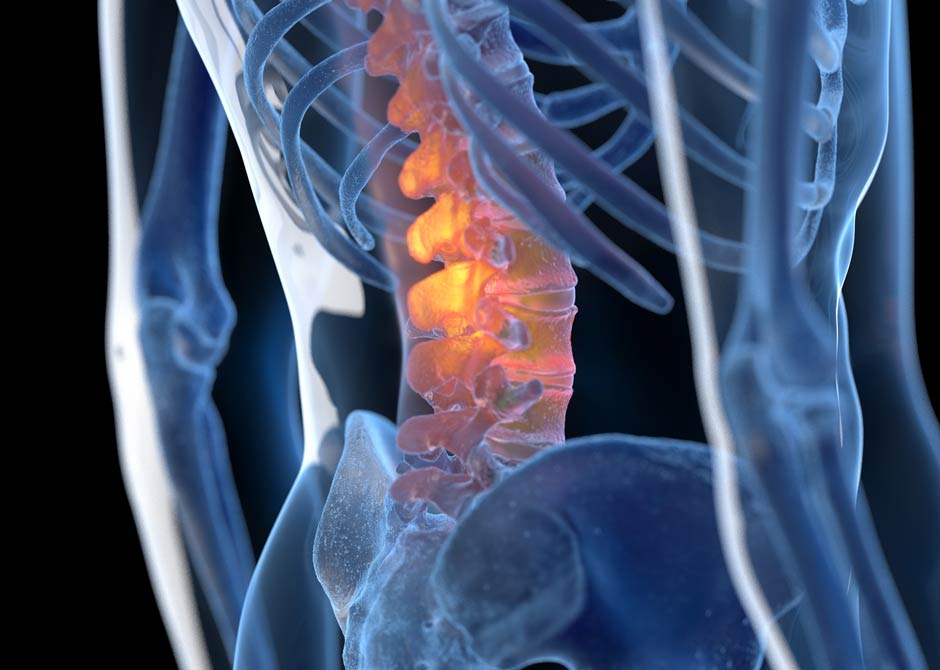
Facet joint syndrome, also known as facet joint arthritis or osteoarthritis, is a condition characterized by pain in the facet joints of the spine. Facet joints are small, paired joints located on the back of each vertebra, linking adjacent vertebrae together and allowing for smooth movement of the spine. These joints are lined with cartilage and surrounded by a capsule filled with synovial fluid, similar to other joints in the body.
Facet joint syndrome commonly affects the cervical (neck) and lumbar (lower back) regions of the spine, as these areas are subject to a significant amount of movement and mechanical stress. The condition is typically caused by degenerative changes in the facet joints over time, including wear and tear, cartilage breakdown and the formation of osteophytes (bone spurs).
Other factors such as injury, trauma, poor posture and obesity may also contribute to the development of facet joint syndrome.
What are the symptoms of facet joint syndrome?
Facet joint syndrome typically presents with symptoms localized to the affected area of the spine. Common symptoms include:
- Localized pain: Pain is usually felt in the lower back (lumbar region) or neck (cervical region) and may be described as dull, achy or sharp. The pain may worsen with certain movements or activities that put pressure on the facet joints.
- Stiffness: You may experience stiffness in the affected area, particularly after prolonged periods of inactivity or upon waking in the morning.
- Limited range of motion: Facet joint syndrome can lead to reduced flexibility and difficulty extending, twisting or turning the spine.
- Radiating pain: In some cases, pain from the facet joints may radiate into the buttocks, the hips or down the legs (for lumbar facet joint syndrome) or into the shoulders, arms or hands (for cervical facet joint syndrome).
- Tenderness: The area overlying the affected facet joint may be tender to the touch.
- Muscle spasms: Tightness or spasms in the muscles surrounding the affected facet joint may occur as your body’s response to pain and instability.
Symptoms of facet joint syndrome can vary in intensity and may be worsened by certain activities or positions.
How is facet joint syndrome diagnosed?
The gold standard in diagnosing facet joint pain are medial branch blocks and intra-articular injection of local anesthetics.
- Diagnostic injections: In some cases, your doctor may recommend diagnostic facet joint injections, where a local anesthetic is injected into the facet joint suspected of causing your pain, or diagnostic medial branch blocks, where local anesthetic is injected around the nerve that senses pain from the joint. If the injection provides temporary pain relief (1 to 8 hours), it can confirm the diagnosis of facet joint syndrome.
- Medical history: Your doctor will ask about your symptoms, including the location, duration and severity of pain, as well as any activities or movements that worsen or alleviate your symptoms.
- Physical examination: Your doctor will conduct a physical exam to assess your spine’s range of motion, strength of muscles along the spine and tenderness in the affected area. They may also perform specific maneuvers to reproduce your pain and identify the source.
- Imaging:
- X-rays: These can show changes in the bones and alignment of the spine, such as osteoarthritis, or degenerative changes in the facet joints.
- MRI (magnetic resonance imaging): This provides detailed images of the spine, including soft tissues like ligaments and discs, allowing the doctor to visualize any inflammation or damage to the facet joints.
- CT scan (computed tomography): Sometimes used to provide additional detail, especially if MRI is inconclusive or if there is suspicion of bony abnormalities.
By combining the information from these tests and procedures, we can more accurately diagnose facet joint syndrome and develop an appropriate treatment plan.
How is facet joint syndrome treated?
At Ohio State, we offer nonsurgical and surgical treatment options for facet joint syndrome. This helps alleviate pain, improve function and enhance quality of life for our patients. The choice of treatment depends on factors such as the severity of symptoms, underlying cause of facet joint syndrome and your personal preferences.
Nonsurgical treatment options
- Radiofrequency ablation (RFA): Often the best treatment option, this procedure involves using heat to disrupt the nerve fibers that transmit pain signals from the facet joint, providing long-term pain relief.
- Physical therapy: Targeted exercises and stretches can improve flexibility, strengthen supportive muscles and reduce pressure on the facet joints.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants and pain relievers can alleviate symptoms.
- Steroid injections: For patients with contraindications to RFA, steroid injections directly into the affected facet joint can provide temporary pain relief and reduce inflammation.
Surgical treatment options
While there are surgical options for treating facet joint syndrome, these surgeries are rarely utilized.
- Facet joint fusion: In cases of severe facet joint degeneration or instability accompanied by pinched nerve pain in the arm or leg, fusion surgery may be performed to stabilize the affected vertebrae and reduce pain.
Is facet joint syndrome permanent?
Facet joint syndrome, typically caused by injury or arthritis, can lead to persistent pain and discomfort in the affected area of the spine. While the symptoms of facet joint syndrome can be managed with various treatments such as physical therapy, medication and injections, the underlying damage to the facet joint itself may not be reversible. Therefore, you may require ongoing treatment and management to alleviate symptoms and maintain spinal health.
Spinal Stenosis
How would you like to schedule?
Don’t have MyChart? Create an account
